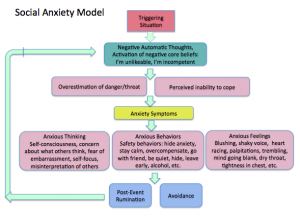
Uncertainty is a part of our every day lives. For some, uncertainty can trigger anxiety. Although cognitive behavior therapy and other interventions are helpful to those with social anxiety and other anxiety disorders, uncertainty can have a negative impact on the effectiveness of those interventions.
One of our therapists, Erica Russell, wrote a blog for the National Social Anxiety Center. Erica dives into the topic of uncertainty and it’s effect on social anxiety. She discusses the various ways that people with social anxiety struggle with uncertainty and strategies to overcome these struggles.
Check out her latest blog post here!