The National Social Anxiety Center supports Naomi Osaka’s decision to take time off to focus on her mental health and well-being. We admire her courage in sharing her own struggle with social anxiety and related depression. In doing so, Ms. Osaka is bringing more awareness to the issue of mental health in sports and the broader struggles of individuals in our society.
Author Archive for Laura Johnson
If you have social anxiety, avoidant coping modes may help you avoid activation of your schemas and your inner critic. Schemas are broad, pervasive themes regarding oneself and others, developed during childhood and reinforced throughout one’s lifetime. They tend to be unhelpful to a significant degree. In social anxiety, schemas may consist of core beliefs related to fear of being judged, criticized by others, or embarrassing oneself. Coping modes such as avoidance often get activated to avoid the pain of the schema.
For many years, you may have been told that your OCD behaviors are too extreme and that you need to wash less and worry less. Now with Covid-19, it seems everyone is washing and worrying. How do you know the difference between healthy behaviors and OCD?
The Covid-19 pandemic may be impacting your OCD symptoms, including your obsessions and/or your compulsions. If this is the case for you, read on for some specific tips based on the type of OCD you have.
If You Struggle with Contamination Fears:
- Develop a basic safety plan based on the recommendations of the Center for Disease Control (CDC) and trusted health professionals, and do not add to it.
- Practice good hand hygiene but don’t overdo it. Wash your hands with soap and water for 20 seconds after being outside or in public, before eating, after going to the bathroom, and after you’ve coughed/sneezed/blown your nose. If soap and water are not available, use hand sanitizer that contains at least 60% alcohol.
- Disinfect surfaces no more than once a day. Focus on the surfaces in your home that are frequently touched, and think about whether this is truly needed (for example, if you stayed home all day and had no visitors, do you really need to disinfect that doorknob?). This process shouldn’t take you more than a few minutes per day.
- If you want to do more than this, ask a friend or family member or your therapist to help you figure out what might be a reasonable and the rational safety measure to take.
If You Struggle with Perfectionism:
- Remind yourself that no one can protect themselves “perfectly” from Covid-19, and no one expects you to. Times like these call for using your common sense instead of going to perfectionistic extremes.
- Remember that trusted health organizations aren’t thinking about people with OCD and/or perfectionism when they set public health guidelines. It might be helpful to talk to a trusted friend, family member, and/or your therapist to help figure out what “common sense” means.
- Your therapist can be especially helpful in figuring out how to apply these guidelines in a way that meets health standards without sending you deeper into your OCD.
If You Struggle with Thoughts of Harming Others:
- Be mindful that your OCD may take advantage of Covid-19 fears by telling you that you might have infected someone or that you are going to infect someone in the future, whether accidentally or on purpose.
- If you’re noticing these intrusive thoughts, or that you’re doing compulsions related to these thoughts, check in with your therapist and let them know how your symptoms might have changed. They can work with you to come up with new exposures and/or homework activities to help contain them.
How To Get Help for OCD
The Cognitive Behavior Therapy Center of Silicon Valley specializes in OCD in adults, children and teenagers. The Silicon Valley office serves the Santa Clara County communities of San Jose, Saratoga, Mountain View, Santa Clara, Sunnyvale, Los Gatos, Los Altos, Palo Alto, Cupertino, Campbell and surrounding areas. Contact us for more information on how we can help you overcome OCD.
In a recent online forum at the Harvard T.H. Chan School of Public Health, Donn Posner, the forum’s featured speaker, said sleep problems are becoming more common and offered tips for falling and staying asleep.
A summary of his speech was published in The Harvard Gazette. His main points were:
- Even though it may seem counterintuitive after a lost night’s sleep, avoid napping, or at least cut it short.
- Do not sleep late on weekends or after a night tossing and turning. Do not to make up for lost sleep because it only interferes further with your bodies natural rhythm.
- You do not have to maintain your former sleep and waking times, which may have been set by the necessities of a daily commute. Keep a rhythm, even if it’s a different time of day than it used to be.
- Once awake, try to get some sunlight, whether by taking a walk or sitting by a window.
- Keep a regular schedule for meals and exercise.
- Avoid stimulants such as caffeine, nicotine, and electronic devices for several hours before bed.
- If sleeps proves impossible, get out of bed. Do something relaxing — read or do a puzzle. Worrying about sleep exacerbates the problem, so try to distract yourself and keep your bed a place of sanctuary.
How to Get Help for Insomnia/Sleep Problems
The Cognitive Behavior Therapy Center of Silicon Valley specializes in sleep problems in adults, children and teenagers. The Silicon Valley office in Los Gatos serves the Santa Clara County communities of San Jose, Saratoga, Mountain View, Santa Clara, Sunnyvale, Los Gatos, Los Altos, Palo Alto, Cupertino, Campbell and surrounding areas. Contact us at (408) 384-8404 for more information on how we can help you overcome sleep problems.
If you have OCD, the messages in the media can be confusing. Your therapist and the OCD literature have been telling you not to wash your hands, to stop checking and to accept uncertainty. Now everyone is saying the opposite and now it seems like it really is a serious risk. How do you know what to do? How do you know when it is your OCD talking and when you are really practicing proper safety protocols? The OCD Foundation has put together some resources to help you. Click here to learn more: Resources for OCD during the Covid-19 Outbreak by the OCD Foundation.
The Cognitive Behavior Therapy Center is offering online Video Therapy that you can do from home. Learn more about our video therapy program. Contact us at (408) 384-8404 or click here to send an email.
The Happiness Trap: How to Stop Struggling and Start Living
Author: Russ Harris
Russ Harris, in his book The Happiness Trap, does a fantastic job of breaking down the concepts of Acceptance and Commitment Therapy (ACT) into digestible and manageable steps in order to untangle from the unworkable control strategies humans use to try to “solve” internal experiences. We all tend to fight “negative” or unwanted internal experiences (i.e., feeling any way uncomfortable) and try to grab hold of something “positive” or wanted; however, we end up feeling even more miserable. The author reviews the myths of happiness and what we do internally to actually make ourselves suffer more in pursuit of it.
This book helps readers accept thoughts and feelings, connect with their values, and take effective actions to live a more meaningful and fulfilling life. It is a great book for anyone who is struggling to find happiness, trapped in a never ending pattern with their thoughts or emotions, struggling with self-esteem, or struggling to get rid of any unwanted discomfort. And as the title states, this book is for anyone who wants to stop struggling and start living.
How to Get Help in San Jose/Los Gatos
The Cognitive Behavior Therapy Center in Silicon Valley specializes in therapy and counseling with adults, children and teenagers. Click to send an email for more information on how we can help you or your family members improve your outlook.
Silicon Valley Communities We Serve
Cognitive Behavior Therapy Center of Silicon Valley offers evidence-based therapy for Anxiety and Obsessive Compulsive Disorder near the following Silicon Valley/San Jose communities:
San Jose Therapy Counseling • Saratoga Therapy Counseling • Los Gatos Therapy Counseling • Monte Sereno Therapy Counseling • Cupertino Therapy Counseling • Campbell Therapy Counseling • Mountain View Therapy Counseling • Los Altos Therapy Counseling • Sunnyvale Therapy Counseling • Santa Clara Therapy Counseling
CONTACT US
Click to send an email
Love Me, Don’t Leave Me: Overcoming Fear and Abandonment & Building Lasting, Loving Relationships
Author: Michelle Skeen
It’s now common to hear things among our communities like “I have abandonment issues,” or “I’m scared of my partner leaving,” but we tend not to think about the core fears (mistrust and abuse, emotional deprivation, defectiveness, and failure) that accompany these statements. The book Love Me, Don’t Leave Me: Overcoming Fear and Abandonment & Building Lasting, Loving Relationships, reviews these core beliefs and includes a short assessment for each, so readers can determine what areas are most problematic for them.
The author not only includes sections on how these core schemas can impact our own behaviors in relationships – and what to do about this, but also a section on what types of people and triggers to be on the lookout for in a partner. This latter part is helpful for anyone trying to take steps to make their own behavior and their relationships more healthy.
After the information-giving part of the book, the author discusses actions you can take to improve behavioral patterns. These actions include catching cognitive distortions, being more present and aware of your actions, focusing on your values instead of unhealthy scripts, being more flexible, and improving communication skills.
How to Improve Your Relationships in San Jose/Los Gatos
The Cognitive Behavior Therapy Center in Silicon Valley specializes in therapy and counseling with adults, children and teenagers. Click to send an email for more information on how we can help you or your family members improve your outlook.
Silicon Valley Communities We Serve
Cognitive Behavior Therapy Center of Silicon Valley offers evidence-based therapy for Anxiety and Obsessive Compulsive Disorder near the following Silicon Valley/San Jose communities:
San Jose Therapy Counseling • Saratoga Therapy Counseling • Los Gatos Therapy Counseling • Monte Sereno Therapy Counseling • Cupertino Therapy Counseling • Campbell Therapy Counseling • Mountain View Therapy Counseling • Los Altos Therapy Counseling • Sunnyvale Therapy Counseling • Santa Clara Therapy Counseling
CONTACT US
CBT Skills and Your Health
In A Positive Outlook May Be Good for Your Health, the New York Times reports that actively enhancing positive emotions can boost your immune system and reduce depression. Studies have shown a link between having a positive outlook and health benefits like lower blood pressure and heart disease, better weight control and healthier blood sugar levels.
CBT Skills that Work
In a research study, participants were encouraged to learn at least three of eight skills and practice one or more each day. The eight skills were:
- Recognize a positive event each day.
- Savor that event and log it in a journal or tell someone about it.
- Start a daily gratitude journal.
- List a personal strength and note how you used it.
- Set an attainable goal and note your progress.
- Report a relatively minor stress and list ways to reappraise the event positively.
- Recognize and practice small acts of kindness daily.
- Practice mindfulness, focusing on the here and now rather than the past or future.
How to Get Help for in San Jose/Saratoga and Sacramento/Roseville
The Cognitive Behavior Therapy Center in Silicon Valley (San Jose/Saratoga) and Sacramento Valley (Roseville) specializes in therapy and counseling with adults, children and teenagers. Call us in Saratoga at (408) 384-8404 or in Roseville at (916) 778-0771 or Click to send an email for more information on how we can help you or your family members improve your outlook.
Silicon Valley and Sacramento Valley Communities We Serve
Cognitive Behavior Therapy Center of Silicon Valley offers evidence-based therapy for Anxiety, Obsessive Compulsive Disorder and Eating Disorders near the following Silicon Valley/San Jose communities:
San Jose Therapy Counseling • Saratoga Therapy Counseling • Los Gatos Therapy Counseling • Monte Sereno Therapy Counseling • Cupertino Therapy Counseling • Campbell Therapy Counseling • Mountain View Therapy Counseling • Los Altos Therapy Counseling • Sunnyvale Therapy Counseling • Santa Clara Therapy Counseling
Cognitive Behavior Therapy Center of Sacramento Valley offers evidence-based therapy for Anxiety, Obsessive Compulsive Disorder (OCD) and Eating Disorders near the following Sacramento Valley and Sierra communities:
Sacramento Therapy Counseling • Roseville Therapy Counseling • Rocklin Therapy Counseling • Granite Bay Therapy Counseling • Lincoln Therapy Counseling • Folsom Therapy Counseling • Citrus Heights Therapy Counseling • El Dorado Hills Therapy Counseling • Loomis Therapy Counseling • Grass Valley Therapy Counseling • Auburn Therapy Counseling
CONTACT US
Saratoga: (408) 384-8404
Roseville: (916) 778-0771
Click to send an email
Cognitive Behavior Therapy Skills to Become More Mindful and Manage Anxiety
Mindfulness meditation has become equated with being mindful. But there are alternate ways to build your mindfulness skills. Here’s a way to use CBT skills to become more mindful and manage worry. Read the New York Times article Achieving Mindfulness at Work, No Meditation Cushion Required on a new approach. Some of the main ideas in the article include:
- Self-Distancing: Talking to yourself as an objective adviser would.
- Reasons Why Bad Thing Won’t Happen: Realize that you’ve already made two unrealistic assumptions: that something will happen, and it will be bad. Next, give yourself three reasons the issue you’re worried about might not happen. Notice that it immediately becomes less stressful, because you just went from “it’s going to happen” to “maybe it will happen, maybe it won’t.”
- Reasons If Bad Thing Happens That It Could be Good: Now give yourself three reasons that, if the situation does turn out bad, good things will happen. Now you’ve gone from thinking “there’s this terrible thing that’s going to happen” to thinking “there’s this thing that may or may not happen, but if it does, it could have both good and bad outcomes.”
How to Get Help for Anxiety in San Jose/Los Gatos and Sacramento/Roseville
The Cognitive Behavior Therapy Center in Silicon Valley (San Jose/Los Gatos) and Sacramento Valley (Roseville) specializes in anxiety therapy and counseling with adults, children and teenagers. Click to send an email for more information on how we can help you or your family members overcome anxiety.
Silicon Valley and Sacramento Valley Communities We Serve
Cognitive Behavior Therapy Center of Silicon Valley offers evidence-based therapy for Anxiety and Obsessive Compulsive Disorder near the following Silicon Valley/San Jose communities:
San Jose Therapy Counseling • Saratoga Therapy Counseling • Los Gatos Therapy Counseling • Monte Sereno Therapy Counseling • Cupertino Therapy Counseling • Campbell Therapy Counseling • Mountain View Therapy Counseling • Los Altos Therapy Counseling • Sunnyvale Therapy Counseling • Santa Clara Therapy Counseling
Cognitive Behavior Therapy Center of Sacramento Valley offers evidence-based therapy for Anxiety, Obsessive Compulsive Disorder (OCD) and Eating Disorders near the following Sacramento Valley and Sierra communities:
Sacramento Therapy Counseling • Roseville Therapy Counseling • Rocklin Therapy Counseling • Granite Bay Therapy Counseling • Lincoln Therapy Counseling • Folsom Therapy Counseling • Citrus Heights Therapy Counseling • El Dorado Hills Therapy Counseling • Loomis Therapy Counseling • Grass Valley Therapy Counseling • Auburn Therapy Counseling
CONTACT US
Here’s a letter one of male teen clients wrote after successful completion of cognitive behavior therapy. It’s a very motivating letter for all ages even adults!
Dear Self,
The engine of my car rumbled when I came here, but the funny thing was that I didn’t even know where I was going. Then my parents said “Remember those scary pictures the kids showed you and you were very scared about that?” and I said “Yeah…” Then they said “we’re going to do something about that so we’re going to take you to a therapist to deal with that and not be scared about them anymore.”
I had a lot of fears about looking at the pictures because if my parents said I was scared, I knew at some point I’d see those pictures again. I thought Saryna would be very mean, and I didn’t want to have to be one of those people lying down on the couch just talking. I was totally unready at first. I just didn’t want to be here when we started talking. Once we came up with the hierarchy list, I was completely not ready for doing anything on that list. For the first few times we did the hierarchy, I thought I could do them, but I knew I couldn’t do anything above a level 5. Especially with a level 10, I would have run away. But the third time I was here, we already started and I said “It was no big deal” afterwards. After that, I knew I could definitely get through all of these. If I were to do the highest thing on the hierarchy list then, I would have never came back here again. Currently, I am 11 years old and I can look at one of the scariest pictures in the world.
“Just do it. Don’t let your dreams be dreams. Just do it.”
This is the quote you should think about when something that you have great anxiety around happens.
The practices here were like the practices I did for the multiplication test I had in 3rd grade. I was practicing my multiplication tables with my mom every day. The day I took the test, I got a really good score – almost 100%. This reminds me of now and the whole year I was here. At the beginning, I was so scared to see the pictures. Now, it’s like the day I took the test. I may have a little anxiety when I see the pictures, but I can do it easily.
I learned that sometimes I go turtle speed and sometimes I go rabbit speed. Just like a band aid, if you go really slow to take it off, it’s really painful. But if you go really fast, it hurts too. If you go at the right speed, it doesn’t hurt as much. I realized this is my own speed. It’s my speed that helps me do things and doesn’t make me scared.
My fear was that I couldn’t handle myself in the dark, and I was constantly waking up and going to my parents’ bed. It has probably been a year and when I compare my new self with my old self, you can see a huge difference in my levels of anxiety.
There were two ways I realized my brain was tricking me. Recently, I have had many bloody noses in the middle of the night and whenever I had them I would usually depend on my parents to stop the bleeding and take care of it, and then I would go to their bed because I was awake and scared. But the latest one I’ve had was a very surprising experience because I handled the bleeding and my nose all by myself, and once I was done, I realized I didn’t need my parents to do it.
My brain was tricking me about that. I was really proud of myself after that happened because my brain would trick me all the time. Another reason why I learned my brain was tricking me, each time we looked at a cut up picture of the characters I was scared of, I realized I was willing to bring it closer to me. From that, I realized my brain was tricking me to be constantly cautious without being willing to try anything uncertain.
So that’s why I have created a character of my own called Mr. Muntz. Mr. Muntz helped me realize every time my brain kept saying “no you can’t do this!” That’s what Mr. Muntz would be saying. So to prevent that from happening, I created another character called Homeyeggagetasaurous Rex. Homeyeggagetasaurous Rex was a combined character of all of my favorite people and fantasy and real life. When I thought of Homeyeggagetasaurous Rex, it helped me realize that I can conquer whatever Mr. Muntz told me because the reckless dinosaur I created helped me think of a silly, cool, and strong personality of myself and I wouldn’t need to worry about anything that I’ve done or will be doing that would make me feel scared and have a really high anxiety level.
So as you can see, you can always try even if you’re scared of doing it. As I said, you should listen to the quote “Just do it. Don’t let your dreams be dreams. Just do it.” so that you can focus on the happy time and not let your worries control you.
Sincerely,
The Boy Whose Dreams Came True
Halloween’s Growing Popularity Can Lead to Social Anxiety
Halloween used to be primarily a kid’s holiday. In recent years, Halloween has transformed from a kid-centric holiday into an $8 billion a year industry for everyone. Two in three adults believe Halloween is a holiday for them and not just kids. Many companies allow, and even encourage employees to wear costumes. Halloween’s creep also extends to pets. Americans will spend $370 million on pet costumes this year, with pumpkin (13%), devil (7%), and hot dog (6%) among the most popular. Halloween is now the second-biggest decorating holiday of the year — right behind Christmas.
Common Worries About Halloween
All this pressure to celebrate Halloween can make some folks downright anxious, especially if you suffer from social anxiety. Besides the fear of ghosts, witches and goblins, adults with social anxiety may suffer from other fears such as:
- Worry and indecision about whether to wear a costume and, if so, what to dress up as
- Fear of being judged for the type of costume you choose
- Depression about not being invited to a Halloween party and thinking that everyone else is having fun except you
- Social awkwardness if you do go to a Halloween party, such as not knowing what to say, being uncomfortable with small talk or comparing your costume to others
- Anxiety about opening the door for trick-r-treaters and having to interact with neighbors and strangers
Easing Your Social Anxiety About Halloween
 So what can you do this year to help ease the Halloween jitters?
So what can you do this year to help ease the Halloween jitters?
First, remember Halloween is about fun. No one really cares what you dress up as. Most people are more focused on showing off their own costume than what you are wearing. Since everyone is so focused on their own costumes and being spooky and silly, they are less likely to care whether you talk or what you say anyway.
Second, remember many people enjoy staying home and watching scary movies on Halloween or just doing nothing and relaxing. Take the pressure off yourself if you do end up spending the evening alone. Plan some fun and enjoyable activities for yourself.
Third, if you stay home and don’t feel like opening the door, you can leave a bowl of Halloween candy on your doorstep with a friendly message so your neighbors know you care. Or you can push yourself to face your anxiety, open the door, and hand out candy. You can say “trick-r-treat” and smile. Or just make a pleasant comment about the kids’ and adults’ costumes.
How to Get Help for Social Anxiety in San Jose/Saratoga and Sacramento/Roseville
The Cognitive Behavior Therapy Center in Silicon Valley and Sacramento Valley specializes in social anxiety therapy and counseling with adults, children and teenagers. Call us in Saratoga at (408) 384-8404 or in Roseville at (916) 778-0771 or Click to send an email for more information on how we can help you or your family members overcome your social anxiety.
Silicon Valley and Sacramento Valley Communities We Serve
Cognitive Behavior Therapy Center of Silicon Valley offers evidence-based therapy for Anxiety, Obsessive Compulsive Disorder and Eating Disorders near the following Silicon Valley/San Jose communities:
San Jose Therapy Counseling • Saratoga Therapy Counseling • Los Gatos Therapy Counseling • Monte Sereno Therapy Counseling • Cupertino Therapy Counseling • Campbell Therapy Counseling • Mountain View Therapy Counseling • Los Altos Therapy Counseling • Sunnyvale Therapy Counseling • Santa Clara Therapy Counseling
Cognitive Behavior Therapy Center of Sacramento Valley offers evidence-based therapy for Anxiety, Obsessive Compulsive Disorder (OCD) and Eating Disorders near the following Sacramento Valley and Sierra communities:
Sacramento Therapy Counseling • Roseville Therapy Counseling • Rocklin Therapy Counseling • Granite Bay Therapy Counseling • Lincoln Therapy Counseling • Folsom Therapy Counseling • Citrus Heights Therapy Counseling • El Dorado Hills Therapy Counseling • Loomis Therapy Counseling • Grass Valley Therapy Counseling • Auburn Therapy Counseling
CONTACT US
Saratoga: (408) 384-8404
Roseville: (916) 778-0771
Click to send an email
What is Introversion?
Introversion is “the state of or tendency toward being wholly or predominantly concerned with and interested in one’s own mental life.” According to the Myers-Briggs inventory, introverts are more likely to think, “I like getting my energy from dealing with the ideas, pictures, memories, and reactions that are inside my head, in my inner world. I often prefer doing things alone or with one or two people I feel comfortable with. I take time to reflect so that I have a clear idea of what I’ll be doing when I decide to act. Ideas are almost solid things for me. Sometimes I like the idea of something better than the real thing.”
Introversion vs. Shyness and Social Anxiety
While studies have estimated that introverts are one-third to one-half of the U.S. population, being social and outgoing is prized in our culture so it can be difficult, even shameful, to be an introvert. Mistaking introversion for shyness is a common error. Introversion is different from shyness and social anxiety. Introverts don’t necessarily feel shy or anxious in social situation, although some do. Introverts need downtime to recharge but many introverts function quite well in social situations and leadership roles.
Bias Against Introversion is Slowly Improving
According to Susan Cain, author of Quiet: The Power of Introverts in a World That Can’t Stop Talking, “Our schools, workplaces, and religious institutions are designed for extroverts, and many introverts believe that there is something wrong with them and that they should try to “pass” as extroverts. The bias against introversion leads to a colossal waste of talent, energy, and, ultimately, happiness.”
Due to the popularity of Cain’s book, “Now people think it’s cool to be an introvert,” said Amy J. C. Cuddy, a social psychologist and associate professor at Harvard Business School quoted in a recent New York Times article about Cain’s Quiet Revolution. She added that at least half her students tell her they have read Ms. Cain’s book. “I love that the students are no longer ashamed,” Cuddy said. It seems Brian R. Little, a professor of psychology at Cambridge University, quoted in a New York Times Op Talk column, agrees, “You could almost say that introversion has become the new cool…there has been a recognition of the quiet strengths of introversion.”
Famous Introverts Who Have Changed The World
Many highly influential engineers and scientists, politicians, business people, actresses, actors and comedians, athletes, singers and musicians, movie producers and directors, writers and others in all fields are introverts. Here are some highly successful introverts who have changed the world with their gifts, to name just a few:
- Albert Einstein
- Mahatma Gandhi
- Bill Gates
- Michael Jordan
- Audrey Hepburn
- David Letterman
- Abraham Lincoln
- Larry Page (co-founder of Google)
- Eleanor Roosevelt
- J.K. Rowling
- Steven Spielberg
- Steve Wozniak (co-founder of Apple)
How Can I Be A Proud Introvert?
On the Quiet Revolution website, you can take an introversion test as well as find stories written by Quiet Revolutionaries, individuals who “embody the spirit of Quiet Revolution: strong yet gentle, firm but kind, they are as indomitable as they are unassuming.” Introverts are careful, reflective thinkers who can tolerate the solitude that idea-generation requires. Introverts form the majority of gifted people. Moreover, it appears that introversion increases with intelligence so that more than 75% of people with an IQ above 160 are introverted. In Susan Cain’s TED Talk, one of the most watched of all time with almost 12 million views, she argues that introverts bring extraordinary talents and abilities to the world and should be encouraged and celebrated.
How To Learn to Thrive as an Introvert
The Cognitive Behavior Therapy Center – Silicon Valley (San Jose/Saratoga) and Sacramento Valley (Roseville) – specializes in therapy and counseling with adults, children and teenagers with introverted personality styles. Click to send an email for more information on how we can help you or your family members succeed in life as a quiet revolutionary.
Silicon Valley and Sacramento Valley Communities We Serve
Cognitive Behavior Therapy Center of Silicon Valley offers evidence-based therapy for Anxiety, Obsessive Compulsive Disorder and Eating Disorders near the following Silicon Valley/San Jose communities:
San Jose Therapy Counseling • Saratoga Therapy Counseling • Los Gatos Therapy Counseling • Monte Sereno Therapy Counseling • Cupertino Therapy Counseling • Campbell Therapy Counseling • Mountain View Therapy Counseling • Los Altos Therapy Counseling • Sunnyvale Therapy Counseling • Santa Clara Therapy Counseling
Cognitive Behavior Therapy Center of Sacramento Valley offers evidence-based therapy for Anxiety, Obsessive Compulsive Disorder (OCD) and Eating Disorders near the following Sacramento Valley and Sierra communities:
Sacramento Therapy Counseling • Roseville Therapy Counseling • Rocklin Therapy Counseling • Granite Bay Therapy Counseling • Lincoln Therapy Counseling • Folsom Therapy Counseling • Citrus Heights Therapy Counseling • El Dorado Hills Therapy Counseling • Loomis Therapy Counseling • Grass Valley Therapy Counseling • Auburn Therapy Counseling
CONTACT US
Cognitive Behavior Therapy Center Designated a Specialty Outpatient Clinic by International OCD Foundation
 The Cognitive Behavior Therapy Center of Silicon Valley and Sacramento Valley has been designated as a Specialty Outpatient Clinic by the International OCD Foundation. A Specialty Outpatient Clinic is defined as:
The Cognitive Behavior Therapy Center of Silicon Valley and Sacramento Valley has been designated as a Specialty Outpatient Clinic by the International OCD Foundation. A Specialty Outpatient Clinic is defined as:
1) A minimum of three, licensed clinicians who maintain a professional membership in the IOCDF working in the same outpatient clinic.
2) These clinicians should have 10 combined years experience treating OCD and related disorders.
3) The identified clinic advertises itself as a facility where the primary focus is on the treatment of OCD and/or related disorders.
https://iocdf.org/clinics/cognitive-behavior-therapy-center-of-silicon-valley/
https://iocdf.org/clinics/cognitive-behavior-therapy-center-of-sacramento-valley/
How to Get Help for OCD in San Jose/Saratoga and Sacramento/Roseville
The Cognitive Behavior Therapy Centerspecializes in Obsessive Compulsive Disorder (OCD) therapy and counseling with adults, children and teenagers. Click to send an email for more information on how we can help you or your family members overcome OCD.
Silicon Valley and Sacramento Valley Communities We Serve
Cognitive Behavior Therapy Center of Silicon Valley offers evidence-based therapy for Anxiety, Obsessive Compulsive Disorder and Eating Disorders near the following Silicon Valley/San Jose communities:
San Jose Therapy Counseling • Saratoga Therapy Counseling • Los Gatos Therapy Counseling • Monte Sereno Therapy Counseling • Cupertino Therapy Counseling • Campbell Therapy Counseling • Mountain View Therapy Counseling • Los Altos Therapy Counseling • Sunnyvale Therapy Counseling • Santa Clara Therapy Counseling
Cognitive Behavior Therapy Center of Sacramento Valley offers evidence-based therapy for Anxiety, Obsessive Compulsive Disorder (OCD) and Eating Disorders near the following Sacramento Valley and Sierra communities:
Sacramento Therapy Counseling • Roseville Therapy Counseling • Rocklin Therapy Counseling • Granite Bay Therapy Counseling • Lincoln Therapy Counseling • Folsom Therapy Counseling • Citrus Heights Therapy Counseling • El Dorado Hills Therapy Counseling • Loomis Therapy Counseling • Grass Valley Therapy Counseling • Auburn Therapy Counseling
CONTACT US
Stories of Hope and Resilience in Mental Health
Read Laura Johnson’s book review of “Same Time Next Week” on Positive Psychology New Daily:
http://positivepsychologynews.com/news/laura-lc-johnson/2015060331717
How to Get Help for Anxiety, OCD and Anxiety-Related Problems
The Cognitive Behavior Therapy Center of Silicon Valley and Sacramento Valley specializes in Anxiety, OCD and Anxiety-Related Problems in adults, children and teenagers. We have two convenient locations to serve you.
The Silicon Valley office in Saratoga serves the Santa Clara County communities of San Jose, Saratoga, Mountain View, Santa Clara, Sunnyvale, Los Gatos, Los Altos, Palo Alto, Cupertino, Campbell and surrounding areas.
The Sacramento Valley office in Roseville serves the Placer County and Sacramento County communities of Sacramento, Roseville, Rocklin, Granite Bay, Lincoln, Folsom, Citrus Heights, El Dorado Hills, Loomis, Auburn, Penryn, Grass Valley, Colfax and surrounding areas.
Email us for more information on how we can help you overcome your anxiety-related problems.
A Fun Day in Nature in Carmel Valley
 On Sunday, May 17, the Cognitive Behavior Therapy Center of Silicon Valley employees and their family members spend the day in the very special nature retreat in the Santa Lucia Preserve. As a team, we enjoyed breakfast in the Hacienda, a hike on the Williams Canyon trail, a picnic by the lake and horseback riding on Garzas trail. As the Founder and Center Director of the Cognitive Behavior Therapy Center, I felt so proud of the personal connections the therapist have made with each other. We call ourselves a “no drama” team because we all get along so well and, when there are issues, we speak honestly and directly to resolve issues so they don’t linger and cause resentment. I asked my team members to tell me what they found most meaningful about their day at the Preserve retreat. Below you can read what they said.
On Sunday, May 17, the Cognitive Behavior Therapy Center of Silicon Valley employees and their family members spend the day in the very special nature retreat in the Santa Lucia Preserve. As a team, we enjoyed breakfast in the Hacienda, a hike on the Williams Canyon trail, a picnic by the lake and horseback riding on Garzas trail. As the Founder and Center Director of the Cognitive Behavior Therapy Center, I felt so proud of the personal connections the therapist have made with each other. We call ourselves a “no drama” team because we all get along so well and, when there are issues, we speak honestly and directly to resolve issues so they don’t linger and cause resentment. I asked my team members to tell me what they found most meaningful about their day at the Preserve retreat. Below you can read what they said.
Some Quotes from Our Therapists about their Experience
 “It was so wonderful to spend the day at with my family and coworkers at such a beautiful place. I definitely feel like I got to see a “hidden gem” of the central coast. I loved that we got to do something we do as a family frequently (hiking) as well as something I haven’t done in many many years (horseback riding). The horseback riding was a little out of my comfort zone but turned out to be so fun. Since it was new to most of us I feel like we all got the hang of it together which was really neat.” – Caitlyn Oscarson
“It was so wonderful to spend the day at with my family and coworkers at such a beautiful place. I definitely feel like I got to see a “hidden gem” of the central coast. I loved that we got to do something we do as a family frequently (hiking) as well as something I haven’t done in many many years (horseback riding). The horseback riding was a little out of my comfort zone but turned out to be so fun. Since it was new to most of us I feel like we all got the hang of it together which was really neat.” – Caitlyn Oscarson
“The retreat allowed me the opportunity to get to know the CBT Center staff in a beautiful, relaxed setting. Every day I go into work, I see firsthand the compassion and dedication the therapists show each of their clients. Through the retreat’s various adventures – hiking, picnicking, and horseback riding – I saw that these characteristics extend far beyond the walls of their offices, not only in their individual personalities, but in their relationships with one another. I look forward to our next outing!” – Laura Belknap
“Having never tried horseback riding before, I was a little anxious, but I got to experience firsthand what my clients experience during exposure. By the end of the ride, my anxiety had dropped way down and riding the horse ended up being my favorite part of the retreat!” -Erica Russell
“Our day at the Preserve was an opportunity to spend time with colleagues and family outside of the office. We have a unique professional environment at the CBT Center where we can challenge each other to grow professionally while also genuinely enjoying each other’s company personally. One of the highlights for me was seeing the impact of restricting public access to a large piece of land. The wildlife had less fear of humans and you could see trees and lush green open spaces for as far as the eye could see. We don’t often think about what a place might look like if preserved in this way, so I found this notably eye-opening.” – Melissa Gould
“I always find it to be very meaningful for me to feel connected with nature, yet I found it most meaningful to become more connected with the CBT team through the shared experiences and getting to meet one another’s loved ones. I think it was a helpful and healthy reminder for me to not get swallowed up by my daily tasks, and to appreciate others’ company and acknowledge my own value of connectedness and need for self-care.” – Saryna Konczey
How to Get Help for Anxiety in San Jose/Saratoga and Sacramento/Roseville
The Cognitive Behavior Therapy Center of Silicon Valley (San Jose/Saratoga) and Sacramento Valley (Roseville) specializes in anxiety therapy and counseling with adults, children and teenagers. Call (408) 384-8404 or Click to send an email for more information on how we can help you or your family members overcome your anxiety-related disorders.
Silicon Valley and Sacramento Valley Communities We Serve
Cognitive Behavior Therapy Center of Silicon Valley offers evidence-based therapy for Anxiety, OCD and Eating Disorders near the following Silicon Valley/San Jose communities:
San Jose Therapy Counseling • Saratoga Therapy Counseling • Los Gatos Therapy Counseling • Monte Sereno Therapy Counseling • Cupertino Therapy Counseling • Campbell Therapy Counseling • Mountain View Therapy Counseling • Los Altos Therapy Counseling • Sunnyvale Therapy Counseling • Santa Clara Therapy Counseling
Cognitive Behavior Therapy Center of Sacramento Valley offers evidence-based therapy for Anxiety, Obsessive Compulsive Disorder (OCD) and Eating Disorders near the following Sacramento Valley and Sierra communities:
Sacramento Therapy Counseling • Roseville Therapy Counseling • Rocklin Therapy Counseling • Granite Bay Therapy Counseling • Lincoln Therapy Counseling • Folsom Therapy Counseling • Citrus Heights Therapy Counseling • El Dorado Hills Therapy Counseling • Loomis Therapy Counseling • Grass Valley Therapy Counseling • Auburn Therapy Counseling
CONTACT US
Call (408) 384-8404 or Click to send an email
An Important Twist on the Mindful Moment by Reid Wilson, Ph.D.
Anxious clients enter treatment in the position of resistance. If they are diagnosed with an anxiety disorder, they’ve got to be resisting. They want that discomfort to go away, which is totally understandable. But the stance of ‘I don’t want this to be happening’ gives Anxiety the upper hand, because the mind & body will move into battle mode. If we teach them permissive skills, like brief relaxation or mindfulness, they are more likely to say, ‘Let me take a mindful stance in this situation. And I hope this works, because I’ve got to get rid of this feeling.’ These skills associated with permitting & accepting the symptoms often allow the client to slide right back into resisting.
Say “Yes” to Anxiety
If clients can truly say ‘yes’ to the encounter, & accept exactly what they are experiencing in that moment, then they will be back in control. This is manifested in the supportive message of ‘It’s OK that I’m anxious, I can handle these feelings, & I can manage this situation.’
It’s a Paradoxical Approach to Anxiety
This approach has a paradoxical flair to it that people often miss. You take actions to manipulate the symptoms while simultaneously permitting the symptoms to exist. With physical symptoms, you are saying, ‘It’s OK that I am anxious right now. I’m going to take some Calming Breaths & see if I settle down. If I do, then great. But if I stay anxious, that’s OK with me, too.’We attempt to modify the symptoms without becoming attached to the need to accomplish the task. This is a critical juncture in the work, & the therapist must track closely the client’s expected move of, ‘I’m going to apply these relaxation skills because I need to relax in this situation.’ No! While it is fine to relax in an anxiety-provoking situation, it is not OK to insist that you relax. That’s how anxiety wins.
Vist http://www.anxieties.com for more self-help strategies on the Anxiety Mental Game.
How to Get Help for Anxiety – San Jose/Saratoga and Sacramento/Roseville
The Cognitive Behavior Therapy Center specializes in anxiety therapy and counseling with adults, children and teenagers. Click to send an email for more information on how we can help you or your family members overcome your anxiety-related disorders.
Silicon Valley and Sacramento Valley Communities We Serve
Cognitive Behavior Therapy Center of Silicon Valley offers evidence-based therapy for Anxiety, OCD and Eating Disorders near the following Silicon Valley/San Jose communities:
San Jose Therapy Counseling • Saratoga Therapy Counseling • Los Gatos Therapy Counseling • Monte Sereno Therapy Counseling • Cupertino Therapy Counseling • Campbell Therapy Counseling • Mountain View Therapy Counseling • Los Altos Therapy Counseling • Sunnyvale Therapy Counseling • Santa Clara Therapy Counseling
Cognitive Behavior Therapy Center of Sacramento Valley offers evidence-based therapy for Anxiety, Obsessive Compulsive Disorder (OCD) and Eating Disorders near the following Sacramento Valley and Sierra communities:
Sacramento Therapy Counseling • Roseville Therapy Counseling • Rocklin Therapy Counseling • Granite Bay Therapy Counseling • Lincoln Therapy Counseling • Folsom Therapy Counseling • Citrus Heights Therapy Counseling • El Dorado Hills Therapy Counseling • Loomis Therapy Counseling • Grass Valley Therapy Counseling • Auburn Therapy Counseling
CONTACT US
Click to send an email
New CBT Center of Anxiety and OCD Opening in Roseville, CA
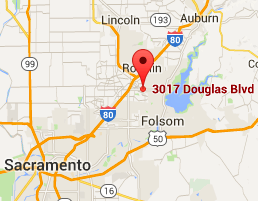 On June 1st, the Cognitive Behavior Therapy Center is expanding to the Sacramento Valley with a new branch office in Roseville, CA. The name of the new office is Cognitive Behavior Therapy Center of Sacramento Valley. With our convenient location on Douglas Boulevard in Roseville just minutes from I-80, the new CBT Center will serve the communities of Sacramento, Roseville, Rocklin, Granite Bay, Lincoln, Folsom, Citrus Heights, El Dorado Hills, Loomis, Penryn, Grass Valley, Colfax, Auburn and surrounding areas.
On June 1st, the Cognitive Behavior Therapy Center is expanding to the Sacramento Valley with a new branch office in Roseville, CA. The name of the new office is Cognitive Behavior Therapy Center of Sacramento Valley. With our convenient location on Douglas Boulevard in Roseville just minutes from I-80, the new CBT Center will serve the communities of Sacramento, Roseville, Rocklin, Granite Bay, Lincoln, Folsom, Citrus Heights, El Dorado Hills, Loomis, Penryn, Grass Valley, Colfax, Auburn and surrounding areas.
Anxiety and OCD Therapy for Adults, Children and Teens in Roseville/Sacramento Valley
At the Cognitive Behavior Therapy Center of Sacramento Valley in Roseville, we will continue to offer high quality and compassionate evidence-based therapy for adults, children and teenagers with anxiety and OCD. The Roseville office will provide therapy for all of the various anxiety disorders including generalized anxiety (GAD), panic disorder, agoraphobia, specific phobias, social anxiety, selective mutism, post-traumatic stress disorder (PTSD), obsessive compulsive disorder (OCD), trichotillomania/hair pulling, skin picking, Tourette Syndrome/tic disorders, eating disorders, and other anxiety-related problems.
Our Current CBT Center in Silicon Valley
The Cognitive Behavior Therapy Center of Silicon Valley currently has a successful anxiety and OCD center in Saratoga, CA, with six therapists and a center assistant serving the San Jose region. We will replicate the high quality of evidence-based services for Anxiety and OCD offered in the Silicon Valley in the Sacramento Valley. The Cognitive Behavior Therapy Centers of Silicon Valley and Sacramento Valley are divisions of Cognitive Behavior Therapy Center, Adult & Child Counseling, Inc. The CBT Center of Sacramento Valley in Roseville will be our second major location.
Contact the Cognitive Behavior Therapy Center of Sacramento Valley
From our office in Roseville just minutes from I-80, we are conveniently located to serve all of Placer County, Sacramento County and surrounding communities. Call (408) 384-8404 or Click to send an email for more information on how we can help you or your family members overcome your anxiety-related issues.
Cognitive Behavior Therapy Center of Sacramento Valley offers evidence-based therapy for Anxiety, Obsessive Compulsive Disorder (OCD) and Eating Disorders near the following Sacramento Valley and Sierra communities:
Sacramento Therapy Counseling • Roseville Therapy Counseling • Rocklin Therapy Counseling • Granite Bay Therapy Counseling • Lincoln Therapy Counseling • Folsom Therapy Counseling • Citrus Heights Therapy Counseling • El Dorado Hills Therapy Counseling • Loomis Therapy Counseling • Grass Valley Therapy Counseling • Auburn Therapy Counseling
CONTACT US
(916) 778-0771 or Click to send an email
Announcing Our Membership in the National Social Anxiety Center
 The Cognitive Behavior Therapy Center • Silicon Valley / Sacramento Valley is proud to announce that we have joined the National Social Anxiety Center, a prestigious alliance of CBT Centers around the country with certified cognitive therapists specializing in evidence-based therapy for social anxiety. Social anxiety (which includes performance anxiety, selective mutism, assertiveness, many types of work anxiety, fear of negative evaluation and judgment and other anxiety-related disorders) is the third most common anxiety disorder in the United States.
The Cognitive Behavior Therapy Center • Silicon Valley / Sacramento Valley is proud to announce that we have joined the National Social Anxiety Center, a prestigious alliance of CBT Centers around the country with certified cognitive therapists specializing in evidence-based therapy for social anxiety. Social anxiety (which includes performance anxiety, selective mutism, assertiveness, many types of work anxiety, fear of negative evaluation and judgment and other anxiety-related disorders) is the third most common anxiety disorder in the United States.
Mission of the National Social Anxiety Center
The mission of the National Social Anxiety Center is to foster effective evidence-based therapy for individuals struggling with social anxiety when the fear of judgment, embarrassment, scrutiny, criticism or rejection inhibits your life.
Regional Centers of the National Social Anxiety Center
The National Social Anxiety Center includes the following regional centers:
NSAC Co-Founders:
John Montopoli, LMFT, LPCC
NSAC San Francisco
http://jmontopolitherapy.com
jrmontopoli@gmail.com
(415) 689-4131
Larry Cohen, LICSW
NSAC Washington DC
Social Anxiety Help
http://www.socialanxietyhelp.com
larrycohen@socialanxietyhelp.com
(202) 244-0903
Regional Founding Members:
Anna Lock, PsyD
NSAC Los Angeles
Behavioral Associates Los Angeles
http://behavioralassociatesla.com
treatment@behavioralassociatesla.com
310-205-0523
Kevin Caridad, LCSW
NSAC Pittsburgh
Cognitive Behavior Institute
http://www.papsychotherapy.org
KevinCaridad.CBI@gmail.com
(724) 609-5002
Laura Johnson, LMFT, LPCC
NSAC Silicon Valley / Sacramento Valley
Cognitive Behavior Therapy Center
https://cognitivebehaviortherapycenter.com
info@cbtsv.com
Saratoga: (408) 384-8404
Roseville: (916) 778-0771
How To Get Help for Social Anxiety in the Silicon Valley / Sacramento Valley
The Cognitive Behavior Therapy Center of Silicon Valley (San Jose/Saratoga) and Sacramento Valley (Roseville) specializes in anxiety therapy and counseling with adults, children and teenagers. Call (408) 384-8404 or Click to send an email for more information on how we can help you or your family members overcome your anxiety-related problems.
Silicon Valley and Sacramento Valley Communities We Serve
Cognitive Behavior Therapy Center of Silicon Valley offers evidence-based therapy for Anxiety, OCD and Eating Disorders near the following Silicon Valley/San Jose communities:
San Jose Therapy Counseling • Saratoga Therapy Counseling • Los Gatos Therapy Counseling • Monte Sereno Therapy Counseling • Cupertino Therapy Counseling • Campbell Therapy Counseling • Mountain View Therapy Counseling • Los Altos Therapy Counseling • Sunnyvale Therapy Counseling • Santa Clara Therapy Counseling
Cognitive Behavior Therapy Center of Sacramento Valley offers evidence-based therapy for Anxiety, Obsessive Compulsive Disorder (OCD) and Eating Disorders near the following Sacramento Valley and Sierra communities:
Sacramento Therapy Counseling • Roseville Therapy Counseling • Rocklin Therapy Counseling • Granite Bay Therapy Counseling • Lincoln Therapy Counseling • Folsom Therapy Counseling • Citrus Heights Therapy Counseling • El Dorado Hills Therapy Counseling • Loomis Therapy Counseling • Grass Valley Therapy Counseling • Auburn Therapy Counseling
CONTACT US
Call (408) 384-8404 or Click to send an email
In the Boston Globe, I read that four smart and talented students at MIT committed suicide within the past year. Among its efforts to help students cope with stress, MIT is encouraging students to talk about the psychological phenomenon called “impostor syndrome,” the feeling of being a failure despite a record of accomplishment.
What is Impostor Syndrome?
Impostor syndrome is common among high achievers, many of whom discount their successes. As a result, they do not feel confident or deserving inside of themselves even though they are objectively successful and perceived as such by other people. Psychological research done in the early 1980s estimated that two out of five successful people consider themselves impostors and other studies have found that 70 percent of all people feel like impostors at one time or another.
The impostor’s thoughts and feelings can be divided into several categories:
1. Feeling like a fake: You may believe that you do not deserve your success, academic standing or professional position. This is accompanied by a fear of being “found out”, “discovered” or “unmasked.” If you feel this way, you might identify with statements such as: “I have tricked other people into thinking that I am more competent than I really am” or “I am often afraid that others will discover I don’t really know what I am doing.”
2. Attributing success to luck: Another aspect of the impostor syndrome is the tendency to attribute success to luck or to other external reasons and not to your own internal abilities. You may refer to an achievement by saying, “I just got lucky this time” or “it was a fluke” and worry you will not be able to succeed next time. You may think you are just lucky, in the right place at the right time, and that’s why you were chosen for a particular job or role.
3. Discounting Success: The third aspect is a tendency to downplay success and discount it. You may discount an achievement by saying “it is not a big deal” or “it was not important.” For example, a student attending a prestigious university may discount the fact that they were accepted or feel like it was a mistake that they were accepted and that they don’t belong or they aren’t as smart as the other students. Or you may say “I did well because it is an easy class” or “I was promoted because my manager left” instead of attributing it to hard work or intelligence. You may also discount your accomplishments and have a hard time accepting compliments.
4. Dwelling on the Negative: You may notice every time where you think you should have done better or where you made a mistake. On the other hand, you overemphasize minor flaws in your performance. You fail to notice, or fail to put enough importance, on what you did well.
5. Unfair Comparisons: You compare yourself unfavorably to others. Frequently you pick out the most outstanding people in your school, company or field and judge your own performance as inadequate and inferior.
Women and Impostor Syndrome
 The term “impostor syndrome” first appeared in an article written by Pauline R. Clance and Suzanne A. Imes in the 1970s. They observed that many high-achieving women tended to believe they were not intelligent, and that they neither internalized nor accepted their own accomplishments. These individuals attributed their successes to luck rather than skill or talent, and were afraid others would realize they’d been deceived by a fraud.
The term “impostor syndrome” first appeared in an article written by Pauline R. Clance and Suzanne A. Imes in the 1970s. They observed that many high-achieving women tended to believe they were not intelligent, and that they neither internalized nor accepted their own accomplishments. These individuals attributed their successes to luck rather than skill or talent, and were afraid others would realize they’d been deceived by a fraud.
While both men and women experience impostor syndrome, studies show that women are more often affected. According to Valerie Young, author of The Secret Thoughts of Successful Women, boys are raised to bluff and exaggerate. Girls, on the other hand, learn early to distrust their opinions and stifle their voices. Young women learn that they tend to be judged by the highest physical, behavioral and intellectual standards. Perfection becomes the goal, and every flaw, mistake or criticism is internalized—slowly reducing self-confidence.
“A real bias against female competence persists,” says Young. “Being female means you and your work automatically stand a greater chance of being ignored, discounted, trivialized, devalued or otherwise taken less seriously than a man’s.”
Sheryl Sandberg, COO of Facebook, spoke of her own feelings of insecurity in her best-selling book, Lean In: Women, Work, and the Will to Lead. When Sandberg attended her Phi Beta Kappa induction at Harvard, a woman gave a speech called “Feeling Like a Fraud.” During the talk, Sandberg looked around the room and saw people nodding. “I thought it was the best speech I’d ever heard,” she recalls. “I felt like that (an impostor) my whole life.” At school, Sandberg thought, “I really fooled them.”
Sandberg says, “Many people, but especially women, feel fraudulent when they are praised for their accomplishments. Instead of feeling worthy of recognition, they feel undeserving and guilty, as if a mistake has been made. Despite being high achievers, even experts in their fields, women can’t seem to shake the sense that it is only a matter of time until they are found out for who they really are – impostors with limited skills or abilities.”
Originally thought to be more common among women, men, too, can be victims of the imposter style of thinking. Even Albert Einstein suffered from impostor syndrome near the end of his life. A month before his death, he reportedly confided in a friend: “the exaggerated esteem in which my lifework is held makes me very ill at ease. I feel compelled to think of myself as an involuntary swindler.”
Do I have Impostor Syndrome?
 Dr. Valerie Young developed the Impostor Syndrome Quiz (reprinted below). If you answer yes to many of these questions, you may have impostor syndrome:
Dr. Valerie Young developed the Impostor Syndrome Quiz (reprinted below). If you answer yes to many of these questions, you may have impostor syndrome:
- Do you secretly worry that others will find out that you’re not as bright and capable as they think you are?
- Do you sometimes shy away from challenges because of nagging self-doubt?
- Do you tend to chalk your accomplishments up to being a “fluke,” “no big deal” or the fact that people just “like” you?
- Do you hate making a mistake, being less than fully prepared or not doing things perfectly?
- Do you tend to feel crushed by even constructive criticism, seeing it as evidence of your “ineptness?”
- When you do succeed, do you think, “Phew, I fooled ‘em this time but I may not be so lucky next time.”
- Do you believe that other people (students, colleagues, competitors) are smarter and more capable than you are?
- Do you live in fear of being found out, discovered, unmasked?
Strategies for Overcoming Impostor Syndrome
1) Become aware of your thoughts. Automatic thoughts can be defined as underlying, unquestioned thoughts, which affect how you perceive an event or situation. Realize them for what they are: negative self-talk that has become a habit. Be aware when you engage in thoughts and feelings of an impostor. Awareness is the first step to change and many times we are not aware of our automatic thoughts.
2) Do a reality check. Question your automatic “impostor” thoughts and feelings and try to come up with more balanced thoughts. Understand the difference between your negative thoughts and reality. Identify the critical voice that is doubting your authenticity. It’s not You. Separate yourself from the critical and self-limiting “impostor” voice.
3) Understand the difference between feelings and reality. Some people believe that if they feel something strongly it must be right. “If I feel so stupid, it must mean that I really am stupid.” When you catch yourself thinking in this way, change it to a coping statement of “the fact that I feel stupid does not mean that I really am. It’s a feeling and not reality.”
4) Write down the steps you took to earn the success you achieved. In one column, make a list of what you accomplished on a particular task or project, and in a second column, write the names of people who helped contribute to the success. Come up with realistic responses that give you credit, but also share praise with others who contributed. For example, you could say to yourself, “I’m proud of what I did on that job, and I had the help of a great team.”
4) Replace your negative “impostor” thinking habit by practicing more realistic and helpful self-talk. Remind yourself of how you contributed to your success with thoughts like “I have proven I am capable by…” or “I prepared for this by…” Give yourself credit throughout the day for both major and minor successes. Notice and reframe “yes, but” statement such as “I brought in accounts but she brought in more” to “Even though she brought in more accounts, I brought in many myself.” Focus on your strengths. When you finish a task, you can ask yourself, “What positive qualities do I have that allowed me to do accomplish this?”
5) Be on the lookout for unhelpful coping strategies you engage in to prevent others from evaluating you negatively. For example, if you tend to hold back from sharing your opinions in meetings, take a risk and speak up in a calm and confident way.
6) Celebrate! Give yourself permission to be proud. Let your friends and family praise you. Take some of it in. Let it touch your heart. Being proud of an accomplishment is not the same as being self-centered. After you celebrate, you will probably remember that no matter what you achieved, chances are there is more to do. This can be humbling and healthy, and important to distinguish from the unhealthy internal put-downs.
7) Give yourself a little time to grow into your success, especially if success seemed to come rather easily or quickly. Sometimes you just need time for a new promotion or status to settle in so you can feel like you deserved it and earned it. However, if you think impostor syndrome is keeping you from getting the most out of your life, then you might want to find a therapist to help you work through your thoughts and feelings.
How To Get Help for Impostor Syndrome
The Cognitive Behavior Therapy Center of Silicon Valley offers counseling and therapy for women and men suffering from Impostor Syndrome. We are located in Saratoga on the border of San Jose and Saratoga just 1/2 mile from Highway 85. With our convenient location near highway 85, we serve the Silicon Valley communities of San Jose, Saratoga, Mountain View, Santa Clara, Sunnyvale, Los Gatos, Los Altos, Cupertino and Campbell, CA. Contact us at (408) 384-8404 for more information on how we can help you savor your accomplishments and reduce your feelings of being an impostor at school or work.
Best Counselor in Saratoga, CA, for Two Years in a Row
The Cognitive Behavior Therapy Center of Silicon Valley has joined the Saratoga Business Hall of Fame by being selected as the Best Counselor for two years in a row. We are honored to have been selected for this prestigious award in 2014 and 2015. We will continue to provide high quality and effective therapy to our clients with Anxiety and Obsessive Compulsive Disorders. We pride ourselves on our passion for CBT and other evidence-based therapies that achieve positive life changes for our clients. Click here to read the press release.
Please contact us at (408) 384-8404 to learn more about our therapy services and to schedule an appointment.
A New Way of Thinking about Coping Styles in Schema Therapy
Cathy Flanagan, one of the original developers of the schema therapy model with its founder, Jeffrey Young, recently published an article in the American Psychological Association’s Journal of Psychotherapy Integration (2014 Vol. 24, No 3, 208-222) where she describes eight modes, or coping styles, that healthy individuals experience. Modes are distinct patterns representing coping strategies to help individuals adapt to situations and to satisfy needs.
In contrast, maladaptive modes or coping styles are extreme forms of normal patterns of adaptation. Each of the eight healthy modes has a corresponding dysfunctional extreme that can become chronically dysfunctional ways of experiencing the self and relating to others.
Healthy and Maladaptive Coping Styles in Schema Therapy
Below are the eight healthy adult modes and the corresponding maladaptive mode that may develop when the strategies are used in excess (the definitions are extracted and summarized from Flanagan’s article).
1. Leader: Behavior, thinking and feelings are all “active.” The Leader is in control, thinking constructively, and openly expressing feelings. Leaders are in touch with both their own needs and the needs of others.
Leader becomes Bully: The Bully operates by demeaning and controlling. Bullies need validation and respect but they elicit hostility and resentment, maintaining a vicious cycle.
2. Caretaker: Caretakers are mentally and physically “on,” and focused on meeting the needs of others. Connection is prioritized and the person’s own needs and feelings come second to those of others.
Caretaker becomes the Martyr: Martyrs do not express their needs but expect that their obvious self-sacrifice will make others respond in kind. The result is a build up of resentment. Martyrs’ excessive need for affirmation induces guilt with the self-defeating effect of making other people pull away.
3. Free Spirit: The Free Spirit actively pursues goals, and reacts in the spirit of the moment. This is a “feel good,” autonomous mode.
Free Spirit becomes Rebel: Rebels have an impulsive, or oppositional style. Rebels’ exaggerated needs for autonomy and change ironically elicit a reaction of correction and control, reinforcing the cycle of rebellion.
 4. Deliberator: Deliberators thoughtfully weigh the possible costs and benefits of different courses of action until a level of certainty is reached. Daydreams and fantasies are entertained for possible action at a later stage.
4. Deliberator: Deliberators thoughtfully weigh the possible costs and benefits of different courses of action until a level of certainty is reached. Daydreams and fantasies are entertained for possible action at a later stage.
Deliberator becomes Worrywart: An excessive need for certainty and an intolerance of ambiguity lead to obsessional thinking and behavioral avoidance. Worrywarts avoid acting or taking risks until they are sure of the outcome. Chronic obsessing or indecision can result in procrastination, reassurance seeking, or resentful dependency.
5. Doer: This mode is defined by action and a single-minded focus on getting a job done or project finished. Doers do not think beyond the task at hand. This can be effective in appropriate doses.
Doer becomes Controller: Controllers are closed to feedback from others. When projects are complete, they go straight to the next one, reaching goals with little sense of satisfaction or connection with other people.
6. Strategizer: Here the pros and cons of various strategies are carefully and dispassionately considered. The focus is on thinking over feelings. Action is suspended until it is considered appropriate or timely.
Strategizer becomes Schemer: For Schemers, life is a battle of wits, a game of chess. This is an impersonal, observing mode. Thinking predominates and results in covert manipulations and passive-aggression. This mode precludes authentic connections with others.
7. Emoter: The Emoter openly expresses his or her feelings, either to get urgent needs met or because the context elicits them. Problem-focused thinking and action are secondary to the immediacy of affect.
Emoter becomes Overreactor: Emotional outbursts, which are intended to elicit validation or reassurance, backfire and can produce rejection or ridicule. Frantic efforts to maintain stability and connection are self-defeating in the same way as a child’s temper tantrum.
8. Follower: This is a “low key” mode. The Follower is content to hand over control. This mode may also represent a period of “down time” or rest. Obviously, not everyone can or should be a Leader so Followers contribute greatly in society.
Follower becomes Victim: This is a markedly passive, subjugated mode where affect is flat, detached, or depressed. Victims need connection, stability, and validation but, by shutting down, the likelihood of getting these needs met is decreased even more.
Therapy Implications for Working with Coping Styles
 This model of healthy and maladaptive coping styles provides opportunities for therapists to consider which tools might be used most effectively with different clients, or at different stages of the therapy process. For example, cognitive reframing, emotional regulation, and behavioral skills training might be strategically utilized to modify certain maladaptive modes. Other tools, such as guided imagery or mindfulness meditation, could be used as appropriate. The point is not so much to specify the exact choice of technique but to target specific mode components with whichever tools are likely to be most effective in the individual case. This will help the client to gradually learn to recognize his/her unhelpful coping styles and to consciously decrease the intensity of these maladaptive components or switch to another, more effective, coping style.
This model of healthy and maladaptive coping styles provides opportunities for therapists to consider which tools might be used most effectively with different clients, or at different stages of the therapy process. For example, cognitive reframing, emotional regulation, and behavioral skills training might be strategically utilized to modify certain maladaptive modes. Other tools, such as guided imagery or mindfulness meditation, could be used as appropriate. The point is not so much to specify the exact choice of technique but to target specific mode components with whichever tools are likely to be most effective in the individual case. This will help the client to gradually learn to recognize his/her unhelpful coping styles and to consciously decrease the intensity of these maladaptive components or switch to another, more effective, coping style.
How to Get Help to Improve Your Coping Styles
The Cognitive Behavior Therapy Center of Silicon Valley offers schema therapy to help you develop more effective coping styles. We are located in Saratoga on the border of San Jose and Saratoga just a 1/2 mile from Highway 85. With our convenient location near highway 85, we serve the Silicon Valley communities of San Jose, Saratoga, Mountain View, Santa Clara, Sunnyvale, Los Gatos, Los Altos, Cupertino and Campbell, CA. In addition, we offer Online Video Therapy for adults in California who are unable to find a qualified schema therapist in your local community. Call us at (408) 384-8404 to learn more about our schema therapy program.
RO-DBT: Your Path to a More Flexible Life and Joyful Experiences
Laura Johnson, LMFT, LPCC, Center Director, attended a two-day workshop on Radically-Open Dialectical Behavior Therapy (RO-DBT) led by its founder, Thomas Lynch, PhD, Professor of Clinical Psychology at the University of Southampton, UK. RO-DBT is an evidence-based approach to help individuals become more flexible in their thinking and responding, more open to life experiences that create joy and happiness, and build intimacy and social connections. RO-DBT can be particularly helpful for individuals with inflexible, rigid personality styles who are susceptible to certain types of anxiety disorders, depression, OCD, perfectionism, anorexia and autism. RO-DBT includes many of the skills taught in traditional DBT but also teaches an entirely new set of skills to increase flexibility and reduce rigidity.
RO-DBT Theory
The theory behind RO-DBT is that children with an “over controlled” temperament are more likely to develop internalizing disorders such as anxiety and depression and become socially isolated as adults. “Overcontrol” is defined as an emotionally constricted, shy and risk averse temperament. In appropriate amounts, overcontrol is a positive trait. You may desire to exceed expectations and perform well, value rules and fairness, delay gratification to achieve goals, and have a high sense of duty, obligation and self-sacrifice.
On the other hand, individuals who develop a excessively overcontrolled style may have a need to appear perfect (planning ahead, being right, stressing orderliness and structure), follow rules (always doing the right thing, being prepared, smiling even when unhappy) and have high pain tolerance (able to work really hard and delay or minimize joy and fun).
Goals of RO-DBT
The goal in RO-DBT is to help individuals develop optimal control that is neither over- or under-controlled.
RO-DBT starts with defining what’s healthy and what’s not. Its interventions strive to build these positive traits including:
- Receptivity and Openness to new experiences (as opposed to high risk aversion, hypervigilance for threat, avoidance of novelty and discounting of constructive feedback)
- Flexible Responding to adapt to changes in the environment (instead of compulsive needs for structure and order, hyper-perfectionism, compulsive planning/rehearsal, and rigid rule-governed behavior)
- Emotional Expression and Awareness to have genuine emotional experiences (as opposed to inhibited expressions or fake expressions and low self-awareness or minimizing of feelings)
- Intimacy and Connection to form long-lasting bonds (instead of aloof/distant relationships, excessive social comparison, envy and bitterness, and low empathy and validation skills)
Ways to Build Flexibility, Openness and Social Connection
In addition to most of the traditional DBT skills, RO-DBT also teaches additional new skills to build the qualities of flexibility, openness and social connection including:
 Radical Openness Skills Module is a completely new skills module where you will learn to change your physiology, engage in new behaviors, learn from constructive feedback, validation skills, build compassion and forgiveness, stimulate positive emotions toward yourself and social connectedness with others through loving kindness meditation,verbal and non-verbal skills to signal openness and friendliness, and communication of emotions to increase social connection and reduce social isolation and loneliness.
Radical Openness Skills Module is a completely new skills module where you will learn to change your physiology, engage in new behaviors, learn from constructive feedback, validation skills, build compassion and forgiveness, stimulate positive emotions toward yourself and social connectedness with others through loving kindness meditation,verbal and non-verbal skills to signal openness and friendliness, and communication of emotions to increase social connection and reduce social isolation and loneliness.
Mindfulness Skills to recognize when you are in fixed mind vs. fatalistic mind and how to get to flexible mind and to teach self inquiry.
Emotion Regulation Skills to reduce envy, bitterness, resentment and revenge.
Some Examples of RO-DBT Skills
There are three steps involved in building the skill of Radical Openness:
- Acknowledge the presence of unwanted or uncomfortable feelings such as irritation, tension in the body, negative emotions or feelings of uncertainty
- Turn toward the discomfort and use Self-Inquiry to ask yourself, “What do I need to learn from this?” instead of automatically distracting or accepting
- Flexibly Respond by doing what’s needed in the moment
Practicing being open to feedback from others includes the following steps:
- Acknowledge the feedback
- Describe your emotions, sensations, thoughts and images
- Be Open to new information by cheerleading yourself, adopting an open body stance, and fully listening to the feedback
- Pinpoint what the new behavior is and confirm
- Try out the new behavior
- Self-soothe and reward yourself
How To Get Help in Building Flexibility and Other Positive Traits
The Cognitive Behavior Therapy Center of Silicon Valley specializes in helping individuals change unhelpful thinking and coping styles and build flexibility, openness and social connection. With our convenient location just a half mile from Highway 85 and the Saratoga Avenue exit, we serve the Silicon Valley communities of San Jose, Saratoga, Mountain View, Santa Clara, Sunnyvale, Los Gatos, Los Altos, Cupertino and Campbell, CA. We also have a CBT Online Video Therapy Program for clients in California who live to far away to drive for our specialized therapy in person. Contact us at (408) 384-8404 for more information on how we can help you manage you become more flexible, open and joyful.
By Caitlyn Oscarson, LMFT and Erica Russell, LPCC, LMFT
OCD Foundation’s Behavior Therapy Training Institute 2015
 From January 30th to February 1st, we had the pleasure of attending the International OCD Foundation’s Behavior Therapy Training Institute at UCLA. The Behavior Therapy Training Institute (BTTI) is an intensive three-day training for clinicians who are treating clients with Obsessive Compulsive Disorder. As one of the most prestigious training opportunities for OCD treatment providers, limited space was available, so we both felt very lucky and honored to be in attendance. The faculty of the training included some of the nation’s most well-respected experts in OCD treatment, including Dr. Alec Pollard, Dr. Gerald Tarlow and Dr. John Piancentini. It also included special presentations on pharmacotherapy (or medical treatment) and behavioral therapy for tic disorders, by Dr. Jamie Feusner and Dr. Susanna Chang.
From January 30th to February 1st, we had the pleasure of attending the International OCD Foundation’s Behavior Therapy Training Institute at UCLA. The Behavior Therapy Training Institute (BTTI) is an intensive three-day training for clinicians who are treating clients with Obsessive Compulsive Disorder. As one of the most prestigious training opportunities for OCD treatment providers, limited space was available, so we both felt very lucky and honored to be in attendance. The faculty of the training included some of the nation’s most well-respected experts in OCD treatment, including Dr. Alec Pollard, Dr. Gerald Tarlow and Dr. John Piancentini. It also included special presentations on pharmacotherapy (or medical treatment) and behavioral therapy for tic disorders, by Dr. Jamie Feusner and Dr. Susanna Chang.
The training began with an overview of the assessment and diagnosis of OCD and other OC Spectrum Disorders (Hoarding Disorder, Body Dysmorphic Disorder, Trichotillomania (Hair-Pulling) Disorder and Excoriation Disorder (Skin-Picking Disorder) and then focused in more intensively on treatment approaches.
Exposure and Response Prevention (ERP)
Our clients who are being treated for OCD are probably familiar with the term “exposure and response prevention” (ERP), which involves purposely exposing oneself to an obsession trigger and then preventing any compulsive behaviors or thought actions that might neutralize anxiety. One of the most helpful topics discussed at the training was the importance of approaching obsession triggers in the appropriate way during exposure and having a clear plan for response prevention. We learned that in order for exposure to be as effective as possible, clients should approach obsession triggers in a manner that eliminates all avoidance, neutralization or distraction. This means that if an individual did an exposure involving touching a doorknob, to increase the effectiveness of that exposure it would be important for the individual to not only touch the knob, but then rub his hands on his body and agree not to do any hand-washing or hand-isolating for a specified period of time. It also means that the individual would want to be sure not to have any source of distraction or reassurance that might reduce his anxiety, since experiencing the anxiety and allowing it to decline naturally is what exposure is all about.
Re-Exposure is the Key
The experts also raised the importance of finding creative ways to re-expose if anything interrupts an exposure. For example, if the client who did the doorknob exposure needed to use the restroom and thus had a legitimate reason to wash his hands, it would be important for him to re-expose himself by touching that doorknob again after washing. When doing an exposure to something outside of your home, it can also be helpful for clients with contamination OCD to carry a “contamination rag”, which is a piece of cloth that you would use to wipe whatever surface or substance to which you exposed yourself. That way, if you go home and have reason to wash your hands, you can immediately re-expose yourself to the earlier exposure by wiping the contamination rag on your hands and body.
How to Cope with Anxiety and Distress During Exposures
Another question that often comes up with our clients being treated for OCD is how to cope with the anxiety and distress that can arise during exposures. The OCD experts explained that any coping strategy that helps you engage in exposure can be helpful as long as it doesn’t promote avoidance from feared situations or get in the way of learning new things about the OCD triggers. Ideal strategies will “take the edge off” your anxiety enough to help you engage in the exposure exercise without distracting you from confronting your fears. Therefore, there are no universally “bad” or “good” types of coping strategies. Some suggested strategies such as diaphragmatic breathing and mindfulness are probably familiar to you. Another recommended strategy is to create coping statements or scripts that reflect your beliefs and values and remind you that is it okay to be uncertain. It can also be helpful to focus on all the reasons you want to work on OCD so you feel motivated to participate in exposures.
The Role of Distraction
Some clients ask if it is okay to use distraction techniques, that is, ignoring an upsetting thought, situation or trigger, and focusing your attention on something like reading, talking to a friend, doing a task around the house, watching TV etc. The experts at the BTTI emphasized that distraction won’t help you learn new ways of coping with your OCD, but it also won’t make anything worse in the meantime. So, while it would not be recommended to use distraction all the time, it can be a helpful way to cope with triggers outside of designated exposure time.
How To Get Help for OCD
The Cognitive Behavior Therapy Center of Silicon Valley specializes in Obsessive Compulsive Disorder (OCD) in adults, children and teenagers. With our convenient location just a half mile from Highway 85 and the Saratoga Avenue exit, we serve the Silicon Valley communities of San Jose, Saratoga, Mountain View, Santa Clara, Sunnyvale, Los Gatos, Los Altos, Cupertino and Campbell, CA. We also have a CBT Online Video Therapy Program for clients in California who live to far away to drive for our specialized therapy in person. Contact us at (408) 384-8404 for more information on how we can help you manage you OCD.
I just returned from a two-day Schema Therapy Workshop at the New Jersey Institute for Schema Therapy. The training was led by Wendy Behary, the Founder and Director of The Cognitive Therapy Center of New Jersey and The New Jersey Institute for Schema Therapy and President of the International Society of Schema Therapy. While I have been using Schema Therapy concepts with some clients already, I gained a new appreciation for the complexity, depth and effectiveness of this approach. Starting in March 2015, I am participating in the Advanced Intensive Schema Therapy Training Program. In this article, I will explain some of the basics of schema therapy. Stay tuned for a lot more to come as I work through the intensive training program and get certified!
What is Schema Therapy?
Schema Therapy is an evidence-based approach for long lasting change in the personality dynamics that impact chronic emotional and relationship problems. Schema Therapy was developed by Jeffrey Young while he was at the Beck Institute for Cognitive Behavior Therapy and he eventually branched out on his own. Schema Therapy is considered an integrative model because it draws on cognitive therapy, behaviorism, attachment theory, emotion-focused and relationship-based therapies and other schools of thought. Due to its strong roots in cognitive behavior therapy, I believe it is a natural extension to CBT for helping people who want or need a more depth-oriented approach.
Schema Therapy places emphasis on:
- Identifying and resolving self-defeating life patterns and deeply rooted emotional themes,
- Building resiliency and productive responses to life challenges,
- Drawing out and enabling the strong part of your personality,
- Employing a variety of cognitive, behavioral and emotional change techniques, and
- Using the therapeutic relationship as a vehicle for change
What Is the Theory Behind Schema Therapy?
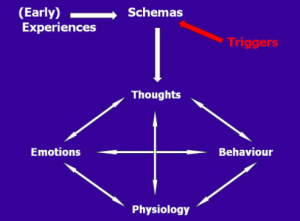 In Schema Therapy, you will learn which of your schemas are triggered when you notice a strong reaction in yourself. The schema model has identified 18 schemas, typically developed when core emotional needs are not meet in childhood. Some common schemas include abandonment, defectiveness/shame, unrelenting standards, and vulnerability to harm/illness.
In Schema Therapy, you will learn which of your schemas are triggered when you notice a strong reaction in yourself. The schema model has identified 18 schemas, typically developed when core emotional needs are not meet in childhood. Some common schemas include abandonment, defectiveness/shame, unrelenting standards, and vulnerability to harm/illness.
In order to cope with the pain when our schemas are triggered, we may develop certain coping styles including:
- Surrender: giving in to our schemas and repeating them over and over,
- Avoidance: finding ways to escape or block out our schemas, and/or
- Overcompensation: doing the opposite of what our schemas make us feel.
When triggered, we may have a strong emotional reaction or mood shift, and we then enter a coping state called a “mode.” There are four categories of schema modes: the innate Child modes (vulnerability, anger, undisciplined/impulsive, contented), the Maladaptive Coping modes (detachment, compliance, overcompensating), the Maladaptive Parent modes (punitive, demanding/critical), and the Healthy Adult mode. The goal of schema therapy is to help you get your core needs met in an adaptive manner by enhancing the Healthy Adult coping mode so your schemas are triggered less frequently and intensely and you can recover more quickly.
Is Schema Therapy Evidence-Based?
I was impressed and pleasantly surprised by the large and growing research base, primarily led by therapists in Europe, where there is support and government funding for longer-term therapies that have been proven effective for deeper and longer-lasting change. In the U.S., most research grants and insurance funding are targeted toward shorter-term therapy approaches for symptom reduction. As a result, schema therapy is not well-known in the U.S. As of this writing, there are no Certified Schema Therapists in California. I hope to change this.
Who Does Schema Therapy Help?
 Schema Therapy is particularly well suited for adults who:
Schema Therapy is particularly well suited for adults who:
- Have recurring depression, anxiety and relationship problems and don’t understand why they stay stuck in the same patterns year after year,
- Want deeper, more long lasting personality change and relapse prevention after their anxiety, depression and other immediate crises have been resolved,
- Have chronic anxiety, OCD and depression that does not respond fully to standard CBT, DBT and exposure therapy protocols, or
- Have successfully completed evidence-based treatment for anxiety, depression, OCD and other problems and want to continue to work on underlying issues in order to improve the quality of their lives and relationships.
Schema Therapy is beginning to be tailored for many populations including children, teens and families. This is an exciting development in Schema Therapy because it will help children and teens develop into healthy adults and prevent them from having chronic anxiety, depression and other problems in adulthood.
What Does Schema Therapy Entail?
Phase 1: Assessment and Education
The assessment phase generally lasts for five to seven sessions and focuses on:
- Education about the Schema Therapy model.
- Assessing schemas and coping styles through interviews, inventories and emotional techniques.
- Scoring and interpreting the results of various schema inventories.
- Activating schemas using emotional techniques such as imagery.
- Noticing how schemas show up in the therapy relationship.
Phase 2: Schema Therapy Treatment
As a longer-term, depth-oriented treatment approach for chronic emotional and relationship problems as well as personality change, you can expect the active treatment phase to be about one to two years of weekly therapy. As mentioned earlier, Schema Therapy uses a variety of strategies to contribute to change.
- Cognitive Techniques: schema diaries, pros and cons of schemas and coping styles, schema dialogues and flashcards.
- Emotion-Focused Techniques: emotional change through imagery, role plays and two-chair work.
- Therapy Relationship: empathic confrontation and analyzing schemas when triggered in sessions.
- Behavioral Techniques: behavioral assignments, skills training and exposure tasks to overcome avoidance of trigger situations.
How to Get Started with Schema Therapy
I hope this article has wet your appetite to learn more about Schema Therapy and perhaps even partake in Schema Therapy yourself. To learn more about Schema Therapy in a self-help format, you can read Reinventing Your Life. If you are interested in starting Schema Therapy, contact the Cognitive Behavior Therapy Center of Silicon Valley at (408) 384-8404 or the Cognitive Behavior Therapy Center of Sacramento Valley at (916) 778-0771 or send us an email.
Note: This article was first published on Positive Psychology News Daily on August 25, 2014
Counseling Psychology is Positive and Strength-Based
Many psychotherapists across many different theoretical models and client populations are already using a positive, strength-based approach to therapy. I was fortunate to graduate from Santa Clara University’s Counseling Psychology Program. The courses were diverse and included positive psychology, health psychology, mindfulness-based stress reduction, cognitive behavior therapy and multicultural counseling, to name just a few. For me, integrating my preferred therapy style, cognitive behavior therapy, with positive psychology felt natural. I often scratch my head about the division between psychotherapy and positive psychology. I believe an effective therapist not only wants to alleviate pain and suffering, but also optimize well-being and functioning. I don’t want clients just to survive. I want to help them thrive.
What is Counseling Psychology?
A core component of Counseling Psychology is, and always has been, its strength-based client focus. According to the Society of Counseling Psychology (division 17 of the APA):
“Counseling Psychology is a specialty within professional psychology that maintains a focus on facilitating personal and interpersonal functioning across the life span…The practice of Counseling Psychology encompasses a broad range of culturally-sensitive practices that help people improve their well-being, alleviate distress and maladjustment, resolve crises, and increase their ability to function better in their lives. With its attention to both normal developmental issues as well as problems associated with physical, emotional, and mental disorders, the specialization holds a unique perspective in the broader practice-based areas of psychology.”
How Do Counseling Psychology and Clinical Psychology Differ?
To contrast the two disciplines, clinical psychologists have tended to focus on psychopathology and clients suffering from more severe mental illnesses while counseling psychologists tend to focus on overall well-being through the lifespan and folks who are experiencing less severe symptoms. For example, Donald Super noticed that clinical psychologists tend to focus their attention on “what is wrong and how to treat it,” whereas counseling psychologists look for “what is right and how to help use it.”
How Therapists Use Client Strengths in Therapy
While there are several theoretical models describing positive, strength-based processes in therapy, there is a scarcity of rigorous scientific studies about how to use positive therapeutic processes in psychological treatment. Scheel, David & Henderson (2012) conducted a small study of eight therapists using a variety of theoretical models in order to identify positive processes that regularly occur in mainstream therapy. The results of the study showed that these therapists recognize the importance of positive processes in therapy and use client strengths to affect therapeutic change.
Gelso and Woodhouse define the use of client strengths as involving two aspects of therapy:
- Conceptualization process (discovering strengths): a) asking questions about client strengths, b) strengths revealed through the therapeutic relationship, c) strengths embedded in client deficits and d) being able understand meaning and expression of strengths within the client’s cultural context.
- Therapist enactments (what therapists actually do that uses clients’ strengths in the change process): a) pointing out strengths to the client, b) positive reframing of strengths, and use of strengths to solve problems, and c) attending to strengths embodied in defenses and perceived deficits.
Cognitive Behavior Therapy (CBT) Focuses on the Positive Processes
Let me quote James Harbin and colleagues:
“CBT interventions focus not only on decreasing negative behaviors but also on increasing positive behaviors…Consistent with strength-based approaches, then, cognitive-behavioral therapists may purposefully encourage client progress to reinforce their hard work in therapy. Strength-based approaches can also be incorporated into goal setting and cognitive restructuring techniques often used in CBT.”
Five General Themes
In-depth interviews with the eight therapists conducted by Scheel, Davis & Henderson (2012) produced 266 significant statements related to how therapists identify and incorporate strengths in the therapy process.
This leads to five themes and associated interventions:
| Theme | Definition | Tools used |
| Amplification of Strengths | A therapeutic process where positive aspects of the client and his/her context are emphasized |
|
| Contextual Considerations | When and how to use client strengths |
|
| Strength-Oriented Processes | Therapy experiences that identify, develop, emphasize and refine strengths |
|
| Strength-Oriented Outcomes | Using client strengths to increase their motivation to want to make changes in their life |
|
| Positive Meaning Making | Narratives clients provide about their past life experiences and how they coped with their difficulties |
|
Advantages of Focusing on Strengths in Therapy
Therapists described strengths work as having many advantages. It was perceived as building trust in the therapeutic relationship, motivating and instilling hope in the client, and demonstrating the therapist’s hope for and belief in the client. In addition, the use of client strengths in therapy is thought to increase client cooperation and acceptance of therapy, and to prevent other problems, promote human growth, and maximize human potential.
A Call for Science
In conclusion, there is a great need for scientific efforts to support and develop evidence-based treatments incorporating positive therapeutic processes. According to Gelso & Woodhouse (2012), “the promotion of human strengths and assets is nowhere more prevalent than in the field of counseling psychology, yet scientific inquiry is needed to advance strength-oriented practices in psychological treatment.”
Resources:
Gelso, C. J. & Woodhouse, S. (2003). Toward a positive psychology: Focus on human strength. In B. W. Walsh (Ed.), Counseling psychology and optimal human functioning (pp. 171-197). Mahwah, NJ: Lawrence Erlbaum Associates.
Harbin, J. M., Gelso, C. J. & Perez Rojas, A. E. (2013). Therapist work with client strengths: Development and validation of a measure. The Counseling Psychologist, XX(X), 1-29.
Scheel, M. J., Davis, C. K., & Henderson, J. D. (2012). Therapist use of client strengths: a qualitative study of positive processes. The Counseling Psychologist, XX(X), 1-36. Society of Counseling Psychology (division 17 of the APA)
Super, D. E. (1977). The identity crisis of counseling psychologists. The Counseling Psychologist, 7, 13-15.
Photo Credits via Compfight with Creative Commons licenses:
Tree of Strengths courtesy of RichardStep.com
Move, Change, Adapt courtesy of RichardStep.com
Umbrella courtesy of Purple Sherbet Photography
You courtesy of RichardStep.com
Exposure and Response (Ritual) Prevention for Obsessive Compulsive Disorder (OCD)
 I recently attended intensive training in Exposure and Response Prevention for OCD at the Center for the Treatment and Study of Anxiety at the University of Pennsylvania in Philadelphia. In addition to terrific presentations by Dr. Elna Yadin, OCD Clinic Director, and staff members, we were honored with a Q&A session with Dr. Edna Foa. While I already considered myself a skilled therapist in treating OCD, this training helped refine my skills in systematically implementing a specialized form of OCD treatment called “Exposure and Response (Ritual) Prevention,” also know as EX/RP or ERP.
I recently attended intensive training in Exposure and Response Prevention for OCD at the Center for the Treatment and Study of Anxiety at the University of Pennsylvania in Philadelphia. In addition to terrific presentations by Dr. Elna Yadin, OCD Clinic Director, and staff members, we were honored with a Q&A session with Dr. Edna Foa. While I already considered myself a skilled therapist in treating OCD, this training helped refine my skills in systematically implementing a specialized form of OCD treatment called “Exposure and Response (Ritual) Prevention,” also know as EX/RP or ERP.
What is Obsessive Compulsive Disorder (OCD)?
Obsessive compulsive disorder (OCD) is a neurological disorder that causes severe anxiety/distress and affects your thinking and behavior. OCD tends to attack the things you value the most. When you feel anxious, it might feel like you are in danger. OCD tells you to respond, react, protect yourself, and do something to get rid of the distress. You might recognize that the fear is excessive or doesn’t make sense, yet it still feels very real, intense, and true. If you have OCD, the warning system in your brain is not working correctly. Your brain is telling you that you are in danger when you are not.
Common Types of OCD
Obsessions are unwanted, intrusive thoughts, images, or impulses that occur over and over again and feel out of your control. They are disturbing, anxiety-provoking and perhaps even disgusting to you. Common obsessions include contamination from germs, bodily fluids, diseases, or chemicals; causing or failing to prevent harm to others; fear of losing control; sexual, religious or morally offensive thoughts and images; perfectionism; and not-just-right feelings.
Compulsions are repetitive behaviors or mental rituals that you engage in to neutralize, undo or make your anxiety go away. Compulsions can also include avoiding situations that trigger obsessions. Common compulsions include checking, washing and cleaning, repeating an action, putting things in order, praying, counting, mental review, reassurance seeking, apologizing and confessing. These actions are designed to prevent or reduce emotional discomfort and avoid the occurrence of a dreaded event. Compulsions tend to provide temporary relief but the obsessions soon return.
It is important to note that OCD comes in many different forms and no two OCD sufferers are alike in their combination of obsessions and compulsions as well as the meaning they attribute to their feared catastrophe.
What is Exposure and Response (Ritual) Prevention (EX/RP)?
In a nutshell, EX/RP consists of exposing you to the triggers that cause anxiety and fear and teaching you to resist doing any compulsions or rituals to reduce the distress. The basic principles of EX/RP can be boiled down to three steps that need to be practiced consistently to overcome OCD:
- Confront the things you fear as often as possible.
- If you feel like you have to avoid something, don’t.
- If you feel like you have to perform a ritual to feel better, don’t.
With EX/RP, your brain learns that you can tolerate anxiety and that your anxiety will eventually come down without rituals. Your brain will learn that the feared catastrophe does not happen or that you could handle it if it did. And you may start to realize just how ridiculous or unrealistic your obsessional fears are and how much OCD is taking away from your life. Basically, OCD is a bully! We will teach you how to take charge and not give OCD the attention it craves.
The main treatment components of EX/RP include:
- Assessment, Education and Treatment Planning: We’ll identify all your triggers, obsessional fears and related rituals and make a plan to systematically approach your fears without engaging in rituals. We will also teach you about the sneaky ways OCD tries to trick you and lies to you. You will learn that OCD is like a “tic” in the brain that is trying to protect you but instead OCD is making you a slave and ruining your life.
- In Vivo Exposure: Exposures are the heart of OCD treatment. In this step, we will expose you to real life triggers that elicit fear, anxiety and/or disgust in a gradual hierarchical manner. We will start with easy exposures and, as you gain confidence you can cope with your anxiety, we will move up the hierarchy to confront situations that are more challenging.
- Imaginal Exposure: This involves prolonged exposure in your imagination to your worst fears without doing any rituals. We’ll develop a script (or series of scripts) for you to record and listen to every day until you are no longer scared of the content of your obsessions and you can visualize yourself facing your fear without any rituals.
- Response (Ritual) Prevention: RP is the identification and elimination of all physical and mental compulsions so you can learn you can cope with distress without doing rituals or avoidance. You will learn that while your rituals reduce anxiety/distress in the short term, they are not building your courage that you can handle anxiety without them. Rituals are actually fuel to OCD’s fire and maintain the OCD cycle.
- Cognitive Processing: The key to long term, permanent change is gaining new beliefs and increasing your self-confidence. OCD is making you believe things that aren’t true and exaggerating the danger of your fears. In order to help you overcome OCD, we won’t tell you what to think because OCD will just argue with you. Instead, we’ll discuss what you have actually learned through your EX/RP activities and reinforce your experiential learning in order to create new beliefs about the meaning of your obsessions.
Treatment Description
In EX/RP, you will purposely experience your obsessive thoughts without ritualizing so you can learn that your discomfort/anxiety will come down and your fear is eventually extinguished. With your therapist, you will develop a hierarchy of exposures that will elicit your obsessional fear and we’ll develop a plan for systematically targeting each of the items. We’ll identify both behavioral and mental rituals to eliminate. EX/RP generally takes about 20 sessions total. We recommend two 75-minute sessions per week to help you maintain continuity and motivation in doing the exposures and to progress more quickly to relieve your suffering.
Initial Evaluation Session
The goal of the initial evaluation session is to learn about your background and history as well as determine what type of anxiety you have. If the diagnosis is OCD, then we will discuss the EX/RP treatment approach and determine if it is a good fit for you. We will also begin to assess your motivation since completing daily exposures in between sessions is essential to success in this program.
Information Gathering and Education
In the next one to two sessions, we will gather a lot of information about the content of your obsessions, types of compulsions/rituals you use to reduce obsessive fears, and the feared consequences if you are unable to perform your rituals. We will use a standardized assessment tool called the YBOCS, which helps us assess all the OCD symptoms and rate the severity of your OCD from mild, moderate to severe. You will also be asked to monitor your OCD symptoms throughout the week. The goal of this phase is to develop a thorough understanding of your obsessions and compulsions and the situations likely to trigger them. We will continue to assess your motivation for treatment and how much support you will need by the therapist and family members in implementing your EX/RP plan.
Treatment Planning
Next, we will spend one to two sessions determining what the feared catastrophe is, creating the hierarchy, identifying and ranking the order of exposures, deciding whether imaginal exposure is needed, creating the plan for reducing and eliminating rituals, and deciding whether exposure requires travel outside the therapist’s office such as a home visit. The question often arises as to whether we need to create different hierarchies for each type of OCD. While this may be helpful when the OCDs seem completely unrelated to one another, it is often not needed because the ultimate fear is often the same for all the OCDs. By creating one master hierarchy and working on fears by level of discomfort/anxiety, you will learn the principles of treatment and the therapy often generalizes more effectively from one symptom to the next.
To create a hierarchy, you and your therapist will generate a list of all the situations that provoke obsessive fear and avoidance behavior. We will then ask you to rate how much distress each situation causes for you on a scale of 0 to 100 and we will place the items in order from easiest to hardest. We generally start working on exposures rated in the 40-50 range and progress to harder exposures and the easier ones are mastered.
Imaginal exposures are used when engaging in the actual situation is not possible in real life, when your feared consequences are so far into the future that they can not be disconfirmed, or when you have so much fear approaching the real life situations that we need to start with thinking about the situation before progressing to actual exposures.
Exposure and Response Prevention Treatment
EX/RP treatment begins when we start working on the first situation on your hierarchy. Generally, 15 exposure sessions are recommended but some people with mild OCD may progress more rapidly while others with more severe OCD may need extra sessions. We will start with doing exposures during the therapy session and then assign the same exposure as homework for you to practice on your own. When your distress significantly declines and you no longer fear the situation, then we will move to the next item on the hierarchy. Since we are starting with items you ranked at a moderate level and only moving up when your distress has declined, it makes working on the harder items on the hierarchy feel much easier. If you find that you are not feeling a reduction of anxiety within 45 minutes, then we have probably underestimated the difficulty of that situation and we would move to an easier item. If we are working at the right pace, you should be feeling challenged in exposure sessions but not so uneasy that you can’t do it.
While doing exposures, you will not be allowed to perform any rituals to undo the anxiety or distress. Sometimes we may allow you to modify a ritual to allow you to approach situations that are more difficult and higher on the hierarchy but our goal will be to quickly eliminate the all rituals associated with that situation. We want your brain to learn that it can face your fears and overcome obsessional fears without doing any rituals.
A key to success in EX/RP is changing how you relate to the meaning of danger created by your OCD. This is called cognitive processing, where we will discuss what you learned from the exposure without doing your normal rituals. We will stress that the content of your obsessions doesn’t matter because OCD will latch onto whatever is important to you. Most people have multiple types of OCD and notice it morphs and evolves over time into new symptoms. We want you to learn the general principles of EX/RP so you can “zap” whatever part of your life OCD wants to target in the future.
We will move up the hierarchy as quickly as you can tolerate it. When all the items on your hierarchy no longer cause distress and you are no longer performing rituals to reduce anxiety, then we can formally end the EX/RP treatment phase.
Relapse Prevention
Generally, we’ll plan on two to three relapse prevention sessions spaced out over time. OCD symptoms often wax and wane with stress and life transitions. Relapse prevention consists of reviewing your progress, identifying the tools you can use to manage any future OCD flare ups, identifying and planning how to handle potential future stressors, and knowing the warning signs of OCD and how you can treat it yourself with your tools, especially self-exposure.
 Hello there. My name is Laura Johnson. I am the founder and director of the Cognitive Behavior Therapy Center of Silicon Valley. I was born in New York and my family moved to Miami when I was four years old. I am multicultural product of an American mother (of Polish and Austrian descent) and a Cuban father, who came to the United States as a teenager.
Hello there. My name is Laura Johnson. I am the founder and director of the Cognitive Behavior Therapy Center of Silicon Valley. I was born in New York and my family moved to Miami when I was four years old. I am multicultural product of an American mother (of Polish and Austrian descent) and a Cuban father, who came to the United States as a teenager.
I went to college at the University of Miami and majored in Advertising Communication. I loved my major because it is the study of what makes people tick and it was creative as well (lots of writing and art classes). After college, I worked for awhile in Miami in market research. Even though I didn’t consider myself very business savvy, I got inspired by some of my colleagues to get an MBA. I only applied to MBA programs out of state because I wanted to gain life experience in another place. Due to my origins in New York, I was thrilled when I got accepted by Columbia University.
I worked for 16 years after getting my MBA in corporate marketing. I spent the first 11 years in brand and product marketing roles for a variety of large companies. I never felt that corporate marketing in big companies was a fit for me due to all the corporate politics and I don’t have the naturally assertive and competitive personality so highly valued in business. I experienced an existential crisis in wondering about my purpose and the meaning of life. I learned about a position developing and leading the Corporate Philanthropy and Employee Volunteerism initiatives where I was working and spent the next 5 years of my career in corporate philanthropy. It was more meaningful and a better fit with my values and personality but it was even more political because everyone wanted to have a say in where we made donations.
While I was still working full time, I decided to explore the field of psychology since my heart had always been in understanding how people think, feel and behave. At first, I considered becoming a career counselor because I thought it would be a good fit with my business background. I applied to Santa Clara University because they had a career counseling program. The Dean encouraged me to also get licensed as a psychotherapist because she said it was hard to survive as just a career counselor. As I started taking psychology classes, I found I absolutely loved it. I had always been reading psychology books anyway and had been in many years of therapy myself.
I knew immediately that I would specialize in cognitive behavior therapy because I had worked with an executive coach/licensed psychologist in the late 1990s on some of my professional issues in the business world. She taught me how to use CBT skills to change my thinking and look at other possible interpretations instead of jumping to conclusions, personalizing and assuming my thoughts were facts. I realized that I had been operating my entire life with a very narrow, biased view of myself and others. I gained a new perspective with CBT and was able to finally feel peace and joy. CBT helped me learn to be satisfied with myself and my life and to be grateful for all my blessings.
After a couple of years working full time and going to school part time at night, I decided to take the plunge and make a 100% commitment to becoming a therapist. I loved psychology so much that I dropped the career counseling courses so I could take more electives in psychology. I figured I knew a lot about business and careers already and I wanted to take classes in health psychology, positive psychology, cognitive behavior therapy and mindfulness.
Since 2005, I have immersed myself in the CBT world by participating in many specialized conferences, advanced workshops and consultation with CBT experts every year in addition to my clinical work. I became interested in specializing in anxiety and OCD during my internship at Kaiser as I noticed that people with anxiety and OCD are the kindest, sweetest and most responsible people who really want to grow and improve. As Kaiser learned about my interest, they directed as many anxiety and OCD cases to me as possible and I co-led several groups for anxious kids and families. By the time I started my individual private practice, I had absolutely no doubt that I would focus on evidence-based CBT for anxiety and OCD with all age groups.
With my passion for CBT and the lack of therapists focusing on evidence-based therapy for anxiety and OCD, I discovered the perfect niche to serve the South Bay area community. As my individual practice grew, I founded the Cognitive Behavior Therapy Center of Silicon Valley. We now have four therapists and an assistant and we moved the office from San Jose to a charming, homey space in Saratoga this year.
 On the personal side, I got married in 2006 to a wonderful, caring man. Since we married later in life, we were not able to have children. However, we have many pets. We have two Cavalier King Charles Spaniels named Rusty and Moon, and two cats – a large black Maine Coon named Frankie and an orange tabby named Sunny. In terms of hobbies, I enjoy reading (I read a lot about psychology in my free time), light jogging, walking, hiking, camping, yoga, and movies. One of my most difficult accomplishments has been maintaining a 70 pound weight loss. It’s not about the numbers but how good I feel now physically and how much more active I have become when I don’t have to lug around the extra weight. For example, I’ve taken up new hobbies in the past few years, like skiing and horseback riding.
On the personal side, I got married in 2006 to a wonderful, caring man. Since we married later in life, we were not able to have children. However, we have many pets. We have two Cavalier King Charles Spaniels named Rusty and Moon, and two cats – a large black Maine Coon named Frankie and an orange tabby named Sunny. In terms of hobbies, I enjoy reading (I read a lot about psychology in my free time), light jogging, walking, hiking, camping, yoga, and movies. One of my most difficult accomplishments has been maintaining a 70 pound weight loss. It’s not about the numbers but how good I feel now physically and how much more active I have become when I don’t have to lug around the extra weight. For example, I’ve taken up new hobbies in the past few years, like skiing and horseback riding.
I work with all age groups and especially love helping children with anxiety and OCD because they change more quickly than adults and I get great satisfaction from knowing I helped “save” a young life from years of unnecessary suffering. I, myself, was a shy, anxious child so I know the pain of feeling different and having low self esteem. Many of my clients say they feel I truly understand their anxiety because of my personal struggles. I am open to sharing small, relevant pieces of my history with my clients when I believe it could be therapeutic. As a cognitive behavior therapist, my greatest joy comes from seeing people have an “aha” moment that changes their life.
My Personal Experience with Cognitive Behavior Therapy
 I’ve had a passion for cognitive behavior therapy (CBT) since the late 1990s when I experienced how broadening my perspective improved my life. I came across CBT in an unusual way. I was attending a four day leadership development seminar. As an introvert, I was struggling in a highly political corporate culture and needed help improving my confidence and relationships at work. Before arriving, I completed a battery of personality tests like the Myers Briggs. On the last day of the seminar, the center brought in a bunch of coaches to help the attendees interpret our results.
I’ve had a passion for cognitive behavior therapy (CBT) since the late 1990s when I experienced how broadening my perspective improved my life. I came across CBT in an unusual way. I was attending a four day leadership development seminar. As an introvert, I was struggling in a highly political corporate culture and needed help improving my confidence and relationships at work. Before arriving, I completed a battery of personality tests like the Myers Briggs. On the last day of the seminar, the center brought in a bunch of coaches to help the attendees interpret our results.
Upon meeting my coach, I admired her presence but thought, “How could she possibly understand me? She looks so confident and at ease in public. She can’t possibly know what it feels like to be nervous to speak up at meetings.” To my surprise, I instantly clicked with her when she shared her experience of being an introvert and how she learned to flex her style to the circumstances. I thought, “If she’s just like me, then there’s hope for me too.” I continued to work with my coach by telephone over the next year and a half.
Fixing My Thinking Traps
My coach listened carefully to how I recounted stories of interactions with colleagues and management. Very early on she said, “I notice you’ve come to a conclusion about what other people are thinking in this situation. You might be right. That’s certainly one conclusion. However, are there any other possibilities of what this situation might mean?” Since my coach approached my beliefs in a supportive and nonjudgmental manner, it melted my resistance and helped me be open to exploring other possibilities.
At first, I didn’t realize that my coach, also a clinical psychologist, was using strategies adapted from cognitive behavior therapy or even what CBT was. She taught me to test my automatic thoughts by identifying all the possibilities of what something might mean and applying percentages to estimate how likely each conclusion was true. I started to see that my initial conclusion might be true but, realistically, it only had about a 30% chance of happening and that there were other logical conclusions I could draw from the same circumstances. I learned to face and plan for my worst fears, like “What if I get fired?” This reduced my anxiety since I no longer thought my “worst case” scenario was 100% true. And, if it did happen, I recognized that I did have the internal resources to cope.
New Perspectives
For example, I might conclude that my manager didn’t value me because she didn’t invite me to a meeting. My coach would say, “Yes, that might be true but are there any others ways to interpret this?” At first this was hard. I’d say, “Well, I really don’t think she values me because a month ago, I didn’t get invited to another meeting.” My coach said, “Okay, but is there any evidence that she does value you?” I thought for a few minutes and said, “Maybe she doesn’t realize I want to be involved with this project because I’ve never shown an interest in it. She probably thinks I’m too busy with all my other work and has decided to take this one on herself. Oh, and now I remember, just last week she gave me a new project and offered to hire a temporary contractor to help me. So I guess she does value me.” The cognitive distortions in my automatic thoughts seem rather obvious now. I was ignoring the positive evidence that my manager valued me and zeroing in on the evidence that supported my negative belief.
Eventually It Becomes More Natural
 Today, the way of thinking I learned from my coach has become more natural and automatic. I’m less likely to jump to conclusions – or when I do – I can stop and ask myself questions to see other possibilities. I continue to actively use CBT skills when I start to feel negative emotions, like worry or anger, in order to manage my mood before it spirals downward. The greatest benefit has been that I feel more engaged in my life and relationships because I’m able to feel subtle positive emotions, like peace and joy. My self-esteem and confidence have increased because I have re-oriented my brain to notice and appreciate the positive, however small it might be.
Today, the way of thinking I learned from my coach has become more natural and automatic. I’m less likely to jump to conclusions – or when I do – I can stop and ask myself questions to see other possibilities. I continue to actively use CBT skills when I start to feel negative emotions, like worry or anger, in order to manage my mood before it spirals downward. The greatest benefit has been that I feel more engaged in my life and relationships because I’m able to feel subtle positive emotions, like peace and joy. My self-esteem and confidence have increased because I have re-oriented my brain to notice and appreciate the positive, however small it might be.
More than a decade later, I am no longer in the corporate world. I went back to school and have become a cognitive behavior therapist, inspired by my personal experience and my desire to help other people find greater peace and joy in their lives.
Note: This article was first published on MentalHelp.net on December 2, 2010.
CBT and Mindfulness for Social Anxiety
Did you know that by practicing cognitive behavioral therapy (CBT) and mindfulness, you can create new circuits in your brain? You can actually change your brain so it’s more flexible, focused and compassionate.
We’ve known for a while that CBT and mindfulness work for many problems especially stress, anxiety and depression. New research is emerging from Stanford University and elsewhere indicating that CBT and mindfulness are effective for social anxiety.
Social Anxiety Model
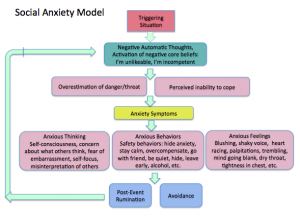 If you have social anxiety, you know that some key problems include negative thinking about yourself, doubt about whether others like or respect you and whether you fit in, and excessive worry and anxiety before, during and after social situations. The model of social anxiety below shows how social anxiety is triggered and maintained. We experience a social or interpersonal situation that activates negative beliefs and assumptions about ourselves or others. Once triggered, we feel anxious because of the negative meaning we’ve given to the situation. We may use “safety behaviors,” or do things that make us feel less anxiety in the moment, but end up making us feel hopeless and discouraged because we don’t learn that we can tolerate anxiety and nothing really bad or scary generally happens. (The exception would be if you are being emotionally, verbally or physically abused or intentionally hurt in some way.) Once social anxiety is triggered, we become self-conscious, worry about what others are thinking, fear being embarrassed, humiliated or looked down on and our self-consciousness causes us to look inward.
If you have social anxiety, you know that some key problems include negative thinking about yourself, doubt about whether others like or respect you and whether you fit in, and excessive worry and anxiety before, during and after social situations. The model of social anxiety below shows how social anxiety is triggered and maintained. We experience a social or interpersonal situation that activates negative beliefs and assumptions about ourselves or others. Once triggered, we feel anxious because of the negative meaning we’ve given to the situation. We may use “safety behaviors,” or do things that make us feel less anxiety in the moment, but end up making us feel hopeless and discouraged because we don’t learn that we can tolerate anxiety and nothing really bad or scary generally happens. (The exception would be if you are being emotionally, verbally or physically abused or intentionally hurt in some way.) Once social anxiety is triggered, we become self-conscious, worry about what others are thinking, fear being embarrassed, humiliated or looked down on and our self-consciousness causes us to look inward.
Changing Your Thoughts
An example might be thinking about going to your high school reunion. You tell yourself, ” No one will remember me. I was such a nerd in high school. The other kids used to make fun of my thick glasses. I really don’t want to go and make a fool of myself again.” You perceive the social danger as rejection. You become self-conscious and focus on yourself and your anxiety reactions. You might predict, “I will end up standing in a corner by myself and no one will talk to me. I’ll make a fool of myself. I’ll feel anxious and won’t be able to stand it.” So you don’t go (safety behavior) and stay home alone with a bottle of wine and ice cream, feeling sad and discouraged.
Imagine, alternatively, if you believed the following: “In high school I was very studious and a few of the jocks made fun of my glasses. I’ve changed now. I’ve grown up, have a good job and people tell me I’m attractive. Even though I didn’t have a lot of friends in high school, I did have a few close friends who may end up going. I would really like to see them. Yes, I might feel anxious in the first half hour or so but I know it’ll pass as I start talking to my friends and having fun.” How might the model of social anxiety change if you had these beliefs instead?
Be a Flexible Thinker
CBT helps you learn more flexible and accurate thinking as well as effective behaviors and coping skills. CBT does not discount the negative but helps you put it into perspective and see what information you might be missing that could help you develop more helpful thoughts and beliefs. Mindfulness can complement CBT by increasing your ability to direct your attention to more productive thoughts and activities and reduce anticipatory anxiety and obsessive rumination.
Note: This article originally appeared on MentalHelp.net on August 16, 2011.
Growing up, I did not consider myself to be a lucky person. I often heard my father saying things like “Everything I buy breaks. I have the worst luck.” When I was nine, I won a holiday raffle at school for a plastic candy cane filled with M&Ms. I was sick that day, the only day I missed that year, and the teacher re-drew names. For years, I saw this as proof I wasn’t lucky. I started to believe, just like my dad, that I had the worst luck and became anxious about trying new things. I expected the worst to happen and my anxious behavior and negative thinking often ensured it did. When things went well, I’d find a reason why it was an exception and when things went poorly, I told myself, “That’s okay. I didn’t expect it to work out anyway.”
 One day when I was in my early 20s, I read a story by a manager explaining his career success. Here’s what I recall him writing:
One day when I was in my early 20s, I read a story by a manager explaining his career success. Here’s what I recall him writing:
“I used to work late every night. One evening, I was in the elevator and the CEO got on. We chatted and he asked me, ‘Haven’t I seen you here before?’ I responded, ‘You might have, sir. I’ve been here every day and evening since I started this job two years ago.’ He said, ‘Son, why don’t you come by my office in the morning.’ The next day,he assigned a tough job to me, one he said needed someone who could work hard and be available to clients at all hours. I gladly accepted and my career progressed over the next 20 years.”
This prompted an “aha” moment. I became inspired to start turning my luck around through hard work and, over time, letting go of my negative inner voice.
Working Hard to Get Lucky
It’s easy to think some people are luckier than others and just “have all the luck” or “are in the right place at the right time.” However, most successful people work hard and, slowly but surely, they encounter and capitalize on lucky opportunities.
Some people do have natural talent and you might think that’s why they are lucky. Have you ever told yourself, “Oh, that person is so lucky but I’ll never amount to anything because I don’t have his or her talent”? It’s easy to fall into this thinking trap when we watch seemingly overnight sensations on reality TV. On the other hand, is that the exception rather than the rule? For example, Michael Grimm, recent winner on “America’s Got Talent,” started working in local bars at age 12. Eighteen years later, it appears he “just got lucky.”
Research has found it takes hard work and deliberate practice, not just natural talent, to achieve great success. Deliberate practice takes your abilities to the next level with disciplined and frequent practice focused on achieving clearly defined objectives, developing specific skills and getting feedback on your performance. Research indicates it takes 10,000 hours, or 10 years on average, of deliberate practice to become an expert in any field.
Your Thinking Can Improve Your Luck
There’s another way to improve your luck. That’s to harness the power of your thinking, attitudes and beliefs about yourself and the world to start noticing opportunities, listening to your intuition, expecting good things to happen and turning bad luck into good luck.
Richard Wiseman’s research, described in The Luck Factor and a Reader’s Digest article, identified four factors common among lucky people. They tend to:
- Be skilled at creating and noticing chance opportunities: Lucky people are relaxed and open to new experiences, allowing them to notice what is present. In contrast, when you are anxious, you may get tunnel vision and miss opportunities.
- Make good decisions by listening to their intuition: Lucky people listen to their inner voice and avoid second guessing themselves too much or looking back on their decisions with regret.
- Create self-fulfilling prophecies with positive expectations: Lucky people expect good things and have an optimistic explanatory style. When bad things happen, lucky people tend to see the cause as external, believe the bad event will end and don’t let it affect too many parts of their life.
- Adopt a resilient attitude that transforms bad luck into good: Lucky people see the positive side of bad events. Instead of telling themselves, “This is awful,” and falling into despair, lucky people focus on how things could have been worse and are thankful for their good luck.
Note: This article originally appeared on MentalHelp.net on September 27, 2010.
CBT Center in the Mercury News
Read about the opening of the Cognitive Behavior Therapy Center of Silicon Valley in the Mercury News.
Chronic Unhappiness is Hard to Change
It’s challenging to try to help people change who have had a lifetime of mental suffering and hold deeply-entrenched negative beliefs about themselves and the world. The other day I was working with a client who yelled out in pain, “There’s nothing positive about my situation!” I sat there feeling helpless because I could see his strengths, but my words fell on deaf ears.
One type of therapy I am exploring for clients with chronic depression is Mindfulness-Based Cognitive Therapy (MBCT), which was developed by Segal, Williams, and Teasdale. They found that people who hold depressive thinking styles are more easily triggered into depressive episodes. The more times this happens, the stronger the neurological connections become and the more likely they are to experience another depressive cycle.
What is MBCT?
MBCT combines mindfulness and cognitive therapy. It is generally taught in an eight-week class of two hours each plus one full-day session. Participants learn mindfulness techniques like the three-minute breathing space, which helps them to call upon mindfulness in stressful moments.
The cognitive therapy component includes learning about negative thinking styles and your own automatic thought patterns, reframing negative thoughts as part of the landscape of depression, recognizing that thoughts aren’t facts and asking yourself questions to help you see reality more clearly. Homework includes using CDs with guided meditations at home.
MBCT in Action
Let’s say you have just gotten chewed out by your boss for turning in a report with several mistakes. Your normal mode of responding might be to defend yourself and argue, “You didn’t give me enough time.” Or maybe it’s to passively listen and then sulk at your desk with thoughts like “I’m no good at this job” and “He’s always such a jerk.” For someone with a strong negative thinking style, this could be enough to trigger depression.
Instead, you can use the three-minute mindful breathing meditation to become aware of the thoughts, feelings, and bodily sensations that arise in the moment of a challenging situation. The goal of the three-minute breathing space isn’t to take away negative feelings. It’s to help you access a clearer frame of mind so you can respond to stressful situations more skillfully and use different approaches to relate to your thoughts.
Promising Research for MBCT
The National Institute for Health and Clinical Excellence in the United Kingdom recommends MBCT for people who are currently well but have experienced three or more depressive episodes. In 2000, a research study found that 66% of participants in MBCT remained relapse-free vs. 34% in the control group. Another study in 2004 replicated the results and found the rate of relapse to be 36% in MBCT group vs. 78% in the control group. MBCT was not found to be effective in people with one or two depressive episodes.
MBCT and Positive Psychology
MBCT has some strategies in common with positive psychology. MBCT helps participants to:
- Observe their negative thoughts with curiosity and kindness
- To accept themselves and stop wishing things were different
- To let go of old habits and choose a different way of being
- To be present in the moment and notice small beauties and pleasures in the world
Just Notice
MBCT is intriguing because the goal isn’t to analyze and change your negative thoughts, but instead to simply be aware of your thoughts and learn to regard them as events of the mind. MBCT teaches people to notice their thought patterns and to change their relationship to their thoughts. Instead of believing the things your mind tells you like, “I am loser because I’ll never get a date,” you might instead just notice, “There’s that thought again that I’m a loser,” without having to react to it.
By noticing when you are at risk of getting caught in the negative habits of your mind, you will be more able to prevent sadness from spiraling into full-blown depression.
References:
Ma, S.H., & Teasdale, J.D. (2004). Mindfulness-based cognitive therapy for depression: Replication and exploration of differential relapse prevention effects. Journal of Consulting and Clinical Psychology, 72, 31-40.
Mindfulness Based Cognitive Therapy sites:
National Institute for Health and Clinical Excellence, United Kingdom. Depression: The treatment and management of depression in adults (see page 10)
Segal, Williams & Teasdale. (2001). Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing RelapseGuilford Press.
Teasdale, J. D., Segal, Z. V., Williams, J. M. G., Ridgeway, V., Soulsby, J., & Lau, M. (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy.. Journal of Consulting and Clinical Psychology, 68, 615-623.
Williams, M., Teasdale, J., Segal, Z. & Kabat-Zinn, J. (2007). The Mindful Way through Depression: Freeing Yourself from Chronic Unhappiness. Guilford Press.
Images
Cycles courtesy of Mike Cattell
Crouching Tiger (butterfly) courtesy of Ajith U
Colorful World of Things Natural (flower) courtesy of sling@flickr
Batur Volcano and Lake (Appreciating Beauty) courtesy of tropicalLiving
Note: This article originally appeared on Positive Psychology News Daily on October 25, 2010. Reprinted with permission of the editors at PPND.
What is Schema Therapy?
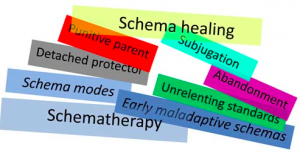 Schema therapy is an extension of cognitive behavior therapy designed to treat a variety of long-standing emotional difficulties with significant origins in childhood and adolescent development. The goal of schema therapy is to help clients get their core needs met in an adaptive manner by enhancing positive schemas and developing healthier coping responses when negative schemas are triggered.
Schema therapy is an extension of cognitive behavior therapy designed to treat a variety of long-standing emotional difficulties with significant origins in childhood and adolescent development. The goal of schema therapy is to help clients get their core needs met in an adaptive manner by enhancing positive schemas and developing healthier coping responses when negative schemas are triggered.
Negative schemas develop when core childhood needs are not met. When parents can more or less meet the child’s core emotional needs in appropriate amounts, the child develops into a healthy adult. Children’s basic needs include:
- Safety
- Stable Base, Predictability
- Love, Nurturing & Attention
- Acceptance & Praise
- Empathy
- Guidance & Protection
- Validation of Feelings & Needs
Schema Therapy vs. Cognitive Behavior Therapy
Compared to traditional cognitive behavior therapy, schema therapy incorporates:
- Greater emphasis on the therapeutic relationship
- More emphasis on affect (e.g., imagery, role-playing) and mood states
- More discussion of childhood origins and developmental processes
- More emphasis on lifelong coping styles (e.g., avoidance and overcompensation)
- More emphasis on entrenched core themes (i.e., core beliefs and schemas)
Schemas — What Are They?
A schema is a stable, enduring negative pattern that develops during childhood or adolescence and is reinforced through thoughts, core beliefs, actions and relationships throughout an individual’s life. We view the world through our schemas. Schemas incorporate core beliefs and feelings about oneself and the environment which the individual accepts without question. They are self-perpetuating, and are very resistant to change.
Even though schemas persist once they are formed, they are not always in our awareness. Usually they operate in subtle ways, out of our awareness. Everyone has schemas since no parent could be a perfect parent and fulfill every emotional need 100% of the time. While the schema descriptions may sound negative, it is normal to have some elements of some schemas within your personality structure. However, when a schema erupts or is triggered by events, our thoughts and feelings are dominated by these schemas. It is at these moments that people tend to experience extreme negative emotions and have dysfunctional thoughts.
18 Common Schema Themes
- Emotional Deprivation: This schema refers to the belief that one’s primary emotional needs will never be met by others. These needs can be described in three categories: Nurturance—needs for affection, closeness and love; Empathy—needs to be listened to and understood; Protection—needs for advice, guidance and direction. Generally parents are cold or removed and don’t adequately care for the child in ways that would adequately meet the above needs.
- Abandonment/Instability: This schema refers to the expectation that one will soon lose anyone with whom an emotional attachment is formed. The person believes that, one way or another, close relationships will end imminently. As children, these clients may have experienced the divorce or death of parents. This schema can also arise when parents have been inconsistent in attending to the child’s needs; for instance, there may have been frequent occasions on which the child was left alone or unattended to for extended periods.
- Mistrust/Abuse: This schema refers to the expectation that others will intentionally take advantage in some way. People with this schema expect others to hurt, cheat, or put them down. They often think in terms of attacking first or getting revenge afterwards. In childhood, these clients were often abused or treated unfairly by parents, siblings, or peers.
- Social Isolation/Alienation: This schema refers to the belief that one is isolated from the world, different from other people, and/or not part of any community. This belief is usually caused by early experiences in which children see that either they, or their families, are different from other people.
- Defectiveness/Shame: This schema refers to the belief that one is internally flawed, and that, if others get close, they will realize this and withdraw from the relationship. This feeling of being flawed and inadequate often leads to a strong sense of shame. Generally parents were very critical of their children and made them feel as if they were not worthy of being loved.
- Failure: This schema refers to the belief that one is incapable of performing as well as one’s peers in areas such as career, school or sports. These clients may feel stupid, inept or untalented. People with this schema often do not try to achieve because they believe that they will fail. This schema may develop if children are put down and treated as if they are a failure in school and other spheres of accomplishment. Usually the parents did not give enough support, discipline, and encouragement for the child to persist and succeed in areas of achievement, such as schoolwork or sport.
- Dependence/Incompetence: This schema refers to the belief that one is not capable of handling day-to-day responsibilities competently and independently. People with this schema often rely on others excessively for help in areas such as decision-making and initiating new tasks. Generally, parents did not encourage these children to act independently and develop confidence in their ability to take care of themselves.
- Vulnerability to Harm and Illness: This schema refers to the belief that one is always on the verge of experiencing a major catastrophe (financial, natural, medical, criminal, etc.). It may lead to taking excessive precautions to protect oneself. Usually there was an extremely fearful parent who passed on the idea that the world is a dangerous place.
- Enmeshment/Undeveloped Self: This schema refers to a pattern in which you experience too much emotional involvement with others – usually parents or romantic partners. It may also include the sense that one has too little individual identity or inner direction, causing a feeling of emptiness or of floundering. This schema is often brought on by parents who are so controlling, abusive, or so overprotective that the child is discouraged from developing a separate sense of self.
- Subjugation: This schema refers to the belief that one must submit to the control of others in order to avoid negative consequences. Often these clients fear that, unless they submit, others will get angry or reject them. Clients who subjugate ignore their own desires and feelings. In childhood there was generally a very controlling parent.
- Self-Sacrifice: This schema refers to the excessive sacrifice of one’s own needs in order to help others. When these clients pay attention to their own needs, they often feel guilty. To avoid this guilt, they put others’ needs ahead of their own. Often clients who self-sacrifice gain a feeling of increased self-esteem or a sense of meaning from helping others. In childhood the person may have been made to feel overly responsible for the well being of one or both parents.
- Emotional Inhibition: This schema refers to the belief that you must suppress spontaneous emotions and impulses, especially anger, because any expression of feelings would harm others or lead to loss of self-esteem, embarrassment, retaliation or abandonment. You may lack spontaneity, or be viewed as uptight. This schema is often brought on by parents who discourage the expression of feelings.
- Unrelenting Standards/Hypercriticalness: This schema refers to the belief that whatever you do is not good enough, that you must always strive harder. The motivation for this belief is the desire to meet extremely high internal demands for competence, usually to avoid internal criticism. People with this schema show impairments in important life areas, such as health, pleasure or self- esteem. Usually these clients’ parents were never satisfied and gave their children love that was conditional on outstanding achievement.
- Entitlement/Grandiosity: This schema refers to the belief that you should be able to do, say, or have whatever you want immediately regardless of whether that hurts others or seems reasonable to them. You are not interested in what other people need, nor are you aware of the long- term costs to you of alienating others. Parents who overindulge their children and who do not set limits about what is socially appropriate may foster the development of this schema. Alternatively, some children develop this schema to compensate for feelings of emotional deprivation or defectiveness. Positive schema to enhance would be empathy and compassion for others.
- Insufficient Self-Control/Self-Discipline: This schema refers to the inability to tolerate any frustration in reaching one’s goals, as well as an inability to restrain expression of one’s impulses or feelings. When lack of self-control is extreme, criminal or addictive behavior rule your life. Parents who did not model self-control, or who did not adequately discipline their children, may predispose them to have this schema as adults.
- Approval-Seeking/Recognition-Seeking: This schema refers to the placing of too much emphasis on gaining the approval and recognition of others at the expense of one’s genuine needs and sense of self. It can also include excessive emphasis on status and appearance as a means of gaining recognition and approval. Clients with this schema are generally extremely sensitive to rejections by others and try hard to fit in. Usually they did not have their needs for unconditional love and acceptance met by their parents in their early years.
- Negativity/Pessimism: This schema refers to a pervasive pattern of focusing on the negative aspects of life while minimizing the positive aspects. Clients with this schema are unable to enjoy things that are going well in their lives because they are so concerned with negative details or potential future problems. They worry about possible failures no matter how well things are going for them. Usually these clients had a parent who worried excessively.
- Punitiveness: This schema refers to the belief that people deserve to be harshly punished for making mistakes. People with this schema are critical and unforgiving of themselves and/or others. They tend to be angry about imperfect behaviors much of the time. In childhood these clients usually had at least one parent who put too much emphasis on performance and had a punitive style of controlling behavior.
At the Cognitive Behavior Therapy Center of Silicon Valley, we have an in-depth interview process and series of questionnaires that can help us identify your primary schemas.
About the Cognitive Behavior Therapy Center of Silicon Valley
The Cognitive Behavior Therapy Center of Silicon Valley offers Schema Therapy for chronic and long standing problems and patterns. With our convenient location just a 1/2 mile from Highway 85 and the Saratoga Avenue exit, we serve the Silicon Valley communities of San Jose, Saratoga, Mountain View, Santa Clara, Sunnyvale, Los Gatos, Los Altos, Palo Alto, Cupertino and Campbell, CA. Contact us at (408) 384-8404 or send an email for more information on how we can help you with long term schema change.
What is Obsessive Compulsive Personality Disorder (OCPD)?
 Obsessive Compulsive Personality Disorder (OCPD) is a type of “personality disorder” with these characteristics:
Obsessive Compulsive Personality Disorder (OCPD) is a type of “personality disorder” with these characteristics:
- Rigid adherence to rules and regulations
- An overwhelming need for order
- Unwillingness to yield or give responsibilities to others
- A sense of righteousness about the way things “should be done”
What are the symptoms of Obsessive Compulsive Personality Disorder (OCPD)?
- Excessive devotion to work that impairs social and family activities
- Excessive fixation with lists, rules and minor details
- Perfectionism that interferes with finishing tasks
- Rigid following of moral and ethical codes
- Unwillingness to assign tasks unless others perform exactly as asked
- Lack of generosity; extreme frugality without reason
- Hoarding behaviors
What is the difference between Obsessive Compulsive Personality Disorder (OCPD) and Obsessive Compulsive Disorder (OCD)
- People with OCD have insight, meaning they are aware that their unwanted thoughts are unreasonable. People with OCPD think their way is the “right and best way” and usually feel comfortable with such self-imposed systems of rules.
- The thoughts, behaviors and feared consequences common to OCD are typically not relevant to real-life concerns; people with OCPD are fixated with following procedures to manage daily tasks.
- Often OCD interferes in several areas in the person’s life including work, social and/or family life. OCPD usually interferes with interpersonal relationships, but makes work functioning more efficient. It is not the job itself that is hurt by OCPD traits, but the relationships with co-workers, or even employers can be strained.
- Typically, people with OCPD don’t believe they require treatment. They believe that if everyone else conformed to their strict rules, things would be fine. The threat of losing a job or a relationship due to interpersonal conflict may be the motivator for therapy. This is in contrast to people with OCD who feel tortured by their unwanted thoughts and rituals, and are more aware of the unreasonable demands that the symptoms place on others, often feeling guilty because of this.
- Family members of people with OCPD often feel extremely criticized and controlled by people with OCPD. Similar to living with someone with OCD, being ruled under OCPD demands can be very frustrating and upsetting, often leading to conflict.
What causes Obsessive Compulsive Personality Disorder (OCPD)?
There is no single, specific “cause” identified. Several theories suggest that people with OCPD may have been raised by parents who were unavailable and either overly controlling or overly protective. Also, as children they may have been harshly punished. The OCPD traits may have developed as a sort of coping mechanism to avoid punishment, in an effort to be “perfect” and obedient.
Therapy for Obsessive Compulsive Personality Disorder (OCPD)
The goal of therapy is to lessen rigid expectations and learn how to value close relationships, recreation, and fun with less emphasis on work and productivity. Therapy can lead to greater insight into how someone’s OCPD symptoms affect others. It often takes the threat of the loss of a relationship or job to motivate people with OCPD seek treatment because they typically don’t think there is anything “wrong” with the way they are. If motivated to change, cognitive behavior therapy, particularly schema therapy, holds much promise.
Getting Help for Obsessive Compulsive Personality Disorder (OCPD)
The Cognitive Behavior Therapy Center of Silicon Valley specializes in long term personality change using CBT and schema therapy. With our convenient location just a 1/2 mile from highways 85 and the Saratoga Avenue exit, we serve the Silicon Valley communities of San Jose, Saratoga, Mountain View, Santa Clara, Sunnyvale, Los Gatos, Los Altos, Palo Alto, Cupertino and Campbell, CA. Contact us at (408) 384-8404 for more information on how we can help you overcome the rigid patterns related to an obsessive compulsive personality.
Many therapists integrate cognitive-behavioral techniques into their therapy approach. However, there are 11 skills that therapists who are experts in CBT try to practice in nearly every session. The list below is from the certification criteria of the Academy of Cognitive Therapy. In order to get certified, therapists must submit an audio tape of a complete session demonstrating competence in all 11 skills. I went a step beyond this and completed the Beck Institute’s full year extramural program where I submitted 46 audiotapes over the year and rated and reviewed each tape with my Beck Institute supervisor. What an amazing experience!
Expert CBT Therapist Skills
1. AGENDA
Your therapist works with you to set an appropriate agenda with target problems, suitable for the available time. Your therapist establishes priorities and follows the agenda. If time is running out, your therapist checks in with you to make sure you want to continue with the current agenda item or move on to the next one.
2. FEEDBACK
Your therapist is adept at eliciting and responding to verbal and non-verbal feedback throughout the session (e.g., elicited reactions to session, regularly checked for understanding, helped summarize main points at end of session).
3. UNDERSTANDING
Your therapist attempts to understand your “internal reality” and is skilled at communicating this understanding to you. Your therapist has excellent listening and empathic skills.
4. INTERPERSONAL EFFECTIVENESS
Your therapist displays optimal levels of warmth, concern, confidence, genuineness, and professionalism.
5. COLLABORATION
Collaboration is excellent. Your therapist encourages you as much as possible to take an active role during the session so you and your therapist can function as a “team.”
6. PACING AND EFFICIENT USE OF TIME
Your therapist used time efficiently by tactfully limiting peripheral and unproductive discussion and by pacing the sessions as rapidly as is appropriate for you.
7. GUIDED DISCOVERY
Your therapist is skillful at using guided discovery during the session to explore problems and help you draw your own conclusions. Your therapist achieves an excellent balance between skillful questioning and other modes of inquiry.
8. FOCUSING ON KEY COGNITIONS OR BEHAVIORS
Your therapist very skillfully focuses on key thoughts, assumptions, behaviors, etc. that are most relevant to the problem area and offers considerable promise for progress.
9. STRATEGY FOR CHANGE
Your therapist follows a consistent strategy for change that seems very promising and incorporates the most appropriate cognitive-behavioral techniques.
10. APPLICATION OF COGNITIVE-BEHAVIORAL TECHNIQUES
Your therapist very skillfully and resourcefully employs cognitive-behavioral techniques.
11. HOMEWORK
Your therapist reviews previous homework and carefully assigns homework for the coming week. Homework assignments are “custom tailored” to help you incorporate new perspectives, test hypotheses, experiment with new behaviors discussed during session, etc.
How To Find an Expert CBT Therapist
The Academy of Cognitive Therapy has an online list of therapists who are certified. You still need to screen the therapists to make sure they are still following the evidence-based CBT model and incorporating the CBT therapist skills. Many therapists get certified and then drift away from the structure and principles of CBT.
Here at the Cognitive Behavior Therapy Center of Silicon Valley, we practice what we preach. If you are interested in getting help for anxiety or OCD with evidence-based CBT, contact us at (408) 384-8404 or send us an email.
 Anxiety is Sneaky
Anxiety is Sneaky
You’re doing fine, and then suddenly you feel like you can’t breathe. Maybe your chest hurts, and you’re convinced you’re having a heart attack. Maybe something happened, like your car won’t start or you heard layoffs might be coming at your company. Or maybe you can’t pinpoint why you are feeling like you are – you woke up in the middle of the night sweating and with a feeling of dread.
You are probably having an anxiety attack — an extreme reaction to stress. Even if you aren’t having a full-blown panic attack, anxiety can leave you feeling apprehensive, uncertain and fearful, paralyzing you with indecision and avoidance.
What is Anxiety?
It’s normal to feel anxious when facing a challenging situation. However, if your worries and fears seem overwhelming and out of proportion with what’s happening and interfere with your daily life, you may be suffering from an anxiety disorder. Common symptoms of anxiety include a surge of overwhelming panic, feelings of losing control or going crazy, a racing heart, heart palpitations or chest pain, feeling like you’re going to pass out, trouble breathing or hyperventilation, trembling or shaking and nausea or stomach cramps. If you have chronic anxiety, you may feel like you are living with constant feelings of apprehension or dread, have trouble concentrating, feel tense or irritable a lot of the time and tend to anticipate the worst.
Anxiety disorders are the most common mental health problems affecting children and adults. According to the Anxiety and Depression Association of America, an estimated 40 million adults (18% of the U.S. population) suffer from anxiety disorders. Only about one-third of those suffering from an anxiety disorder receive treatment, even though anxiety disorders are highly treatable. Below are some steps you can take yourself to manage your anxiety.
10 Steps to Reduce Anxiety, Worry and Stress
1. Get Active. Ride your bike, take a walk, go to a yoga class or go to the gym. There’s no better therapy to reduce the physical sensations of an anxiety attack than to get your blood pumping and endorphins moving through your body with exercise.
2. Cut out all caffeine. Caffeine adds to that tense, jittery, anxious feeling. Sources of caffeine include chocolate, beverages like coffee, tea, soda, and some prescription and over-the-counter medications, like Excedrin.
3. Avoid stressful conversations when you’re tired, overwhelmed, or stressed. For instance, tell your kids that you’re simply not available for problem solving after 8 p.m. Try to protect a “trouble free” time, especially before bed, when you don’t address difficulties but focus instead on pure relaxation.
4. Get sleep. Buy a white-noise machine and use it when you go to sleep. The soothing sound will help you fall and stay asleep. A good night’s sleep is critical when you’re stressed, since sleep deprivation fuels anxiety even as anxiety leads to sleep deprivation.
5. Write about one thing that is making you anxious. Sit down and write out all the fears you have about that one thing. If it’s money, write down what would happen if you lose your job and can’t pay your bills. What is the absolute worst thing that could happen? Now look at each item and mark it on a scale of 1 to 10, with 1 being highly unlikely it would ever happen, 10 being likely that it would happen. You’ll be surprised at how few items rank above a 5. This understanding should help reduce your anxiety. If something does rank higher than 5, you may want to develop a coping plan for it. Nothing works better to calm anxiety than turning from pure worry to an action plan.
6. Practice mindfulness meditation. Relax your body from the toes up. Follow your breath as you observe and detach from your thoughts. Center yourself in the moment (e.g., feel your head upon the pillow, or your feet on the ground, etc.). When your mind wanders, don’t judge it. Simply bring your attention back to your breath.
7. Don’t focus on future problems. Many people get into a cycle of predicting and worrying about future concerns. Ask yourself, “Is this something that could actually happen and, if so, can I do something about it right now?” If the answer to either of these questions is no, tell yourself you will focus on it later. Keep a journal of what makes you anxious. Then revisit these same items when you’re feeling calm and develop plans to deal with them.
8. Experience your anxiety for 45 minutes. That’s usually all it takes for you to become used to it and for the anxious feeling to dissipate. The worst thing you can do is try to ignore your feelings because anxiety tends to fight back if you push it down.
9. Talk to yourself. Remind yourself of how you handled similar situations in the past, your strengths, and how long you will need to get through it. Show yourself that this anxiety is manageable and time-limited.
10. Get busy. Go to the museum, see a movie, read a good book, or take up oil painting (or some other hobby). Rent a comedy and watch it. Let yourself laugh out loud. The act of laughter stimulates endorphins that help blow stress hormones out of your system the way a good thunderstorm can blow away hot, humid weather.
How To Get Help for Your Anxiety
The Cognitive Behavior Therapy Center of Silicon Valley specializes in anxiety, worry and stress in adults, children and teenagers. With our convenient location just a 1/2 mile from highways 85 and the Saratoga Avenue exit, we serve the Silicon Valley communities of San Jose, Saratoga, Mountain View, Santa Clara, Sunnyvale, Los Gatos, Los Altos, Palo Alto, Cupertino and Campbell, CA. Contact us at (408) 384-8404 for more information on how we can help you overcome anxiety, worry and stress.
 How Can You Tell If Your Child is Gifted?
How Can You Tell If Your Child is Gifted?
The process of identifying gifted and talented children is a very complex and highly controversial topic. Much of the available literature focuses on the recognition and identification of intellectually and/or academically gifted children. Schools that have programs for gifted students are often able to identify gifted kids by using traditional screening methods like group IQ tests, review of achievement test scores and past grades, observation, and getting input from teachers and parents. Typically, children identified as intellectually and academically gifted must score at, or above, a specified cutoff score to qualify for educational programming provided by school districts and private organizations. Some school districts also use portfolios and other non-traditional assessments to help identify gifted students, but this varies among states and school districts.
Gifted Children Differ in their Giftedness
Even if you child doesn’t score high enough on intellectual or academic achievement tests, there are many forms of giftedness. If you can answer yes to any of the questions below, your child might be gifted in that particular domain.
- Did your child begin reading before the first day of preschool?
- Is your child extremely talented in the visual and performing arts?
- Does your child exhibit an in depth understanding of math and science?
- Is your child a highly talented swimmer, golfer, or basketball player?
- Does your child display superb public speaking and leadership skills?
Signs Your Child Might Be Gifted
There are no universally accepted traits that you can look for and no definitive signs that will tell you for sure whether your child is gifted. However, many gifted children share some common characteristics, and knowing these is a good place to start.
Language Skills
While most children are able to form recognizable sentences and understand complex language by about two years of age, gifted children often reach these milestones earlier. As they approach school age, other language skills may appear advanced or sophisticated.
Some of the traits of giftedness to look for when considering your child’s language development in relation to others of a similar age include:
- A highly developed vocabulary and the ability to learn new words easily.
- The tendency to speak quickly.
- The early use of longer, more complex sentences while using appropriate grammar.
- Early reading, if given some instruction and opportunity. Many gifted children have already learned how to read before entering school.
- Continually asking questions about what they see and hear, and wanting to receive thorough responses and explanations.
- The ability to understand and carry out multi-step directions at an early age. (e.g., Go to the dining room, get the blue book on the table and put it back on the shelf in your room, then bring me the clothes on your bed so I can wash them).
- The ability to understand and participate in adult conversations. Gifted children often pick up nuances or double meanings early on – so watch what you say!
- The ability to change the language they use when speaking to different audiences. For example, a four-year-old gifted child might use more advanced words and sentence structure when speaking to adults or older children, and then talk in a simpler, more childlike way when addressing his three-year-old cousin.
Learning Abilities
 All children (all people really, big and small) have an inborn desire to learn about the world around them – to seek out new experiences, figure out the relationship between themselves and their surroundings, to discover, and to learn. What distinguishes gifted children from others is the apparent natural ease and joy with which they go about doing this. Their brains appear to be mental sponges, effortlessly absorbing and incorporating new information and ideas.
All children (all people really, big and small) have an inborn desire to learn about the world around them – to seek out new experiences, figure out the relationship between themselves and their surroundings, to discover, and to learn. What distinguishes gifted children from others is the apparent natural ease and joy with which they go about doing this. Their brains appear to be mental sponges, effortlessly absorbing and incorporating new information and ideas.
Many gifted children are natural learners who show some of the following characteristics:
- The ability to learn quickly and efficiently – to pick up ideas and skills effortlessly.
- A tendency to become highly focused on certain areas of interest (e.g., bugs, space, animals) and independently seek out information on these topics.
- The ability to ask questions that show advanced insight or understanding.
- A deep fund of knowledge – they know more about the world around them than you would expect.
- Excellent memory and easy recall of what they previously heard, saw, or learned.
- A tendency to read often on their own and to frequently prefer reading to more physical activities.
- Little need for direction or instruction when beginning a new activity, learning a new game, or acquiring a new skill. They may also insist on doing things on their own, or in their own way.
- Early development of motor skills involving balance, coordination, and movement. Gifted children may also be advanced in some purposeful fine-motor activities such as assembling small objects (e.g., legos, transforming toys, blocks) or putting puzzles together. However, other fine motor skills may not be advanced. Some gifted children are poor at handwriting – although this may be more related to a lack of attention to detail or impatience with the slow and tedious task of handwriting practice than to problems with fine motor control.
- Pleasure in talking to older children and adults about topics that interest them.
- An understanding of their own thinking and learning processes. They may have preferred ways of learning and resist using other methods suggested by a teacher or adult. They are able to sense how much and what kind of studying they need in order to master a skill or topic.
- Creative thinking. Gifted children may enjoy coming up with their own ways to solve problems and take delight in complexity and making connections between seemingly unrelated ideas or concepts.
- The ability to concentrate on a topic of interest for an unusually long period of time. However, gifted children may quickly shift their attention or appear unfocused when doing something they perceive as unchallenging or uninteresting.
- An inclination to see learning as fun. They take joy in discovering new interests or grasping new concepts.
Emotional and Behavioral Traits
Gifted children are often more emotionally intense than others. They can also be more sensitive to others’ feelings and circumstances and may display a great deal of empathy in situations where others their age appear indifferent.
Other emotional or behavioral traits to look for include:
- A high activity level. Gifted children can appear to have an endless source of energy – constantly moving, talking, asking and exploring.
- The tendency to think and talk fast. Because they may be trying to speak as quickly as they think, gifted children are often asked to “slow down” so the listener can understand them. They can also become frustrated when they feel that others are talking too slowly, or taking too long to “get to the point.”
- Strong leadership qualities. Gifted kids often make natural leaders who take charge and lead others in new directions.
- Ability to relate to older kids and adults. Because their cognitive skills and interests can be advanced for their years, gifted kids have an easier time connecting with and learning from those older than themselves.
- Enjoyment of alone time. While gifted children may enjoy spending time with others, including mental mates (whether their own age or adults), they can also enjoy spending time on more solitary activities such as reading, writing, daydreaming, observing, or just thinking.
- Appreciation of natural beauty and art. Gifted children may particularly enjoy being around and pointing out trees, sunsets, flowers, the ocean, animals, and other things of inherent beauty. They can also show a deep interest in certain forms of art – paintings, sculptures, or music, for example.
Hidden Gifts
Some gifted children show only a few of the signs listed above, or show traits that are quite the opposite of what you’d expect. For example, some will start to speak late rather than early, some will be emotionally reserved rather than intense, and some appear to think and speak slowly rather than quickly.
Also keep in mind that there are children who show gifted qualities when it comes to language or emotional traits, but who do not appear exceptional when it comes to learning or academics. While some of these kids may have a specific learning disability getting in the way of their performance at school, others may have learned early on to hide their abilities in order to better fit in with others their age, or to avoid the pressures of higher expectations. And of course there are children who show many of the signs here who do not measure in the gifted range once they are tested. Does that mean they are not gifted? Not necessarily. Many kids don’t shine on IQ tests due to test anxiety – or sometimes because of the very qualities associated with giftedness. For example, IQ tests typically have timed subtests, meaning that the faster a child responds or correctly completes a task, the more points she earns. However, gifted children who are perfectionists may respond more slowly than others, taking their time, working carefully and methodically, and checking their responses for accuracy. A gifted child with a high energy level who has a hard time focusing attention on structured tasks may also be at a disadvantage when it comes to performing in the rigidly structured atmosphere of an IQ test.
In addition, children can be gifted in one area (verbal skills, for example) but show only average ability in others (such as perceptual or nonverbal reasoning skills, which are important for math achievement). While these children’s full-scale IQ score might not measure in the gifted range, they may still demonstrate some common traits of giftedness. For example, a verbally gifted child with average nonverbal reasoning skills may still be emotionally sensitive and have an excellent memory.
Identifying giftedness can be tricky, particularly regarding those who test right around that “magic” cutoff point of 130 or so. And IQ tests are certainly imperfect instruments and only one piece of the puzzle. Your insight and instincts, along with those of your child’s teachers, can often be the most important pieces needed to truly understand your child’s unique gifts and potential.
OCD Quiz: Do You Have Symptoms of Obsessive Compulsive Disorder?
 The following questionnaire will help you identify the types of problems and symptoms that most trouble you. Don’t be surprised if you check more than one item in several groups. Many people have more than one type of OCD symptoms. In addition, OCD can appear in many different forms so it is possible that your particular symptoms are not on this list.
The following questionnaire will help you identify the types of problems and symptoms that most trouble you. Don’t be surprised if you check more than one item in several groups. Many people have more than one type of OCD symptoms. In addition, OCD can appear in many different forms so it is possible that your particular symptoms are not on this list.
Typical OCD Symptoms
What symptoms bothered you? Note how much each item bothered you or interfered with your life in the last month. If you avoided things due to these symptoms, take that into account in your rating. Rate them as follows:
0 = Did not bother me at all /no avoidance due to symptoms / did not interfere with my life
1 = Bothered me a little / some avoidance due to symptoms / interfered with my life a little
2 = Bothered me a moderate amount / avoided several things due to symptoms / interfered with my life quite a bit
3 = Bothered me a lot / avoided many things due to symptoms / significant interference with my life
Washing and Cleaning
___ 1. I avoid touching certain things because of possible contamination.
___ 2. I have difficulty picking up items that have dropped on the floor.
___ 3. I clean my household excessively.
___ 4. I wash my hands excessively.
___ 5. I often take extremely long showers or baths.
___ 6. I’m overly concerned with germs and diseases.
Checking and Repeating
___ 1. I frequently have to check things over and over again.
___ 2. I have difficulty finishing things because I repeat actions.
___ 3. I often repeat actions in order to prevent something bad from happening.
___ 4. I worry excessively about making mistakes.
___ 5. I worry excessively that someone will get harmed because of me.
___ 6. Certain thoughts that come into my mind make me do things over and over again.
Ordering Rituals
___ 1. I must have certain things around me set in a specific order.
___ 2. I spend much time making sure that things are in the right place.
___ 3. I notice immediately when my things are out of place.
___ 4. It is important that my bed is straightened out impeccably.
___ 5. I need to arrange certain things in special patterns.
___ 6. When my things are rearranged by other people, I get extremely upset.
Thinking Rituals
___ 1. Repeating certain words or numbers in my head makes me feel good.
___ 2. I often have to say certain things to myself again and again in order to feel safe.
___ 3. I find myself spending a lot of time praying for non-religious purposes.
___ 4. “Bad” thoughts force me to think about “good” thoughts.
___ 5. I try to remember events in detail or make mental lists to prevent unpleasant consequences.
___ 6. The only way I can stay calm at times is by thinking the “right” things.
Worries and Obsessions
___ 1. I often get upset by unpleasant thoughts that come into my mind against my will.
___ 2. I usually have doubts about the simple everyday things I do.
___ 3. I have no control over my thoughts.
___ 4. Frequently the things that pop into my mind are shameful, frightening, violent, or bizarre.
___ 5. I’m afraid that my bad thoughts will come true.
___ 6. When I start to worry, I cannot easily stop.
___ 7. Little, insignificant events make me worry excessively.
Time Spent on OCD Symptoms
The amount of time you spend on your symptoms is another indication of how much it intrudes in your life. In the past month, how much time have you spent, on an average day, engaged in these symptoms.
Hours/Minutes
________ Washing and Cleaning
________ Checking and Repeating
________ Ordering
________ Thinking Rituals
________ Worrying or Obsessing
________ Total Hours (on an average day)
When to Get Help for OCD
If you find that some symptoms bother you a lot or you are spending more than one hour per day on your symptoms, then you might have a clinical level of OCD. You should see a mental health therapist for an evaluation and possible treatment. The earlier you get help, the better as repeating rituals frequently increases anxiety and OCD.
Where to Get Help for OCD
The Cognitive Behavior Therapy Center of Silicon Valley specializes in obsessive compulsive disorders in adults, children and teenagers. With our convenient location just a 1/2 mile from highways 85 and the Saratoga Avenue exit, we serve the Silicon Valley communities of San Jose, Saratoga, Mountain View, Santa Clara, Sunnyvale, Los Gatos, Los Altos, Palo Alto, Cupertino and Campbell, CA. Contact us at (408) 384-8404 for more information on how we can help you overcome your OCD symptoms.
Source: This OCD Quiz was modified from the questionnaire appearing on anxieties.com.
 When you show up for therapy, it’s natural to assume you are ready to change, right? Otherwise, why would you be paying a therapist to help you work toward a solution? However, sometimes after a few sessions, you may find your motivation is uneven and you aren’t sure you want to do the work involved in getting better and changing your life. That’s where an innovative style of counseling called Motivational Interviewing can help you move through the stages of change.
When you show up for therapy, it’s natural to assume you are ready to change, right? Otherwise, why would you be paying a therapist to help you work toward a solution? However, sometimes after a few sessions, you may find your motivation is uneven and you aren’t sure you want to do the work involved in getting better and changing your life. That’s where an innovative style of counseling called Motivational Interviewing can help you move through the stages of change.
Stages of Change
If you are wondering what’s going on and asking yourself, “Why aren’t I doing the things I know I need to do to get better?,” then you are perfectly normal. Research indicates there are five stages that indicate readiness for change and most people move between them when working on achieving any goal. The five stages of change are:
- Pre-contemplation – you have no intention to take action and may be uninformed about the consequences of your behavior. This is also called “denial” in ordinary language.
- Contemplation – you become aware a problem exists and intend to change but have not yet made a commitment to take action.
- Preparation – you are intending to take action in the next month, may have already tried to change, and may have a plan of action in mind.
- Action – you are beginning to make overt behavioral or environmental changes.
- Maintenance – you are working to prevent relapse and maintain gains.
Strategies Need to Match the Stage You Are In
Most clients, when they first see a professional, are not at the action stage. About 80% are in one of the first three stages and only 20% are in action or maintenance. Resistance to change arises when you and the therapist assume you are in the action stage and start making an action plan to get things done when, in reality, you are not there yet. Instead, it would be better to take a less aggressive approach, acknowledge what stage you are in, and modify homework assignments accordingly.
What Can You Do to Increase Your Readiness to Change?
There is a counseling approach called Motivational Interviewing (MI) that is defined as a “client-centered, directive method for enhancing intrinsic motivation to change by exploring and resolving ambivalence.” In Motivational Interviewing, ambivalence is regarded as a normal part of the change process. MI can increase motivation in the early stages by helping you understand why you want to change. MI can then be followed with cognitive behavioral exercises in the action stage to help you acquire the skills for change.
Principles of Motivational Interviewing
One of the major goals of MI is to help you start thinking about and talking about change before taking action. Talking about your desire and intent to change can be a powerful predictor of change. There are 4 major strategies that the counselor uses to encourage change talk:
- Expressing empathy – using reflective listening to convey understanding of your message.
- Developing discrepancy – between the your most deeply held values and the current behavior you want to change.
- Supporting self-efficacy – building confidence that change is possible.
- Rolling with resistance – meeting resistance with reflection rather than confrontation.
Getting Started with the Process of Change
So even if you are not yet in the action stage, Motivational Interviewing can get you ready for change. If you are interested in reaching a goal this year, maybe the best way to do so is to start with Motivational Interviewing.
How to Get Help in Saratoga/San Jose
The Cognitive Behavior Therapy Center of Silicon Valley offers Motivational Interviewing as a precursor to engaging in action-oriented CBT. The Cognitive Behavior Therapy Center is located at 12961 Village Drive in Saratoga. We are just a 1/2 mile from Highway 85 and the Saratoga Avenue exit. You can contact us (408) 384-8404 for mrs information about how we can help you start the process of change.
 If you are a hard core perfectionist, you’ve probably been criticized at some point for it and your perfectionism might have even annoyed or been intimidating to others. There are lots of advantages to being a perfectionist like striving to do your best, producing great work, being successful, paying attention to details, making fewer errors and being someone people can count on. Some disadvantages of perfectionism include overworking, beating yourself up for making mistakes, never feeling like you are good enough, comparing yourself to others and judging yourself on your performance and other externals. On the other hand, some perfectionists procrastinate because the thought of all the hard work required to do a “perfect” job feels exhausting or they don’t take risks because of fear of failure. When perfectionism gets out of control, it can lead to anxiety and depression.
If you are a hard core perfectionist, you’ve probably been criticized at some point for it and your perfectionism might have even annoyed or been intimidating to others. There are lots of advantages to being a perfectionist like striving to do your best, producing great work, being successful, paying attention to details, making fewer errors and being someone people can count on. Some disadvantages of perfectionism include overworking, beating yourself up for making mistakes, never feeling like you are good enough, comparing yourself to others and judging yourself on your performance and other externals. On the other hand, some perfectionists procrastinate because the thought of all the hard work required to do a “perfect” job feels exhausting or they don’t take risks because of fear of failure. When perfectionism gets out of control, it can lead to anxiety and depression.
Can You Be a More “Perfect” Perfectionist?
You can learn to be an “perfect” perfectionist by keeping the advantages of perfectionism and minimizing the disadvantages. Some strategies like positive reframing, acceptance and humor are the most effective coping skills for dealing with setbacks and helping people feel satisfied at the end of the day. In contrast, some of the least effective coping skills were venting, denial, behavioral disengagement and self-blame. Perfectionists felt worse after using these strategies.
What is Positive Reframing?
Positive reframing involves trying to see things in a more positive light and looking for something good in what happened. Positive reframing, as you’ll see below, is not about turning a negative into a positive but, rather, being able to see reality in a more helpful light. For example, the reframing skill can help you view a setback as a challenge to be overcome or see failure as a learning experience. Reframing is a way of changing the way you look at something and, thus, changing your experience of it. This can relieve stress and help you create a more positive life before you actually start making any changes in your circumstances.
Steps for Reframing a “Failure”
Positive reframing involves four steps:
- Learn about your thinking patterns. Do you tend to fall into the same thinking traps over and over again?
- Notice your thoughts. Catch yourself when you are slipping into overly negative or rigid thinking patterns.
- Examine the truth and accuracy of your negative thoughts. Be a scientist. Ask yourself: What is the evidence for and against this thought? What would I tell a friend? How helpful is it to think this way?
- Develop realistic responses to your negative thoughts about failure and setbacks. If you can’t think of a more positive response, then be more compassionate with yourself, accept the failure and put it into perspective.
If you want to be feel good about yourself and live a more satisfying life, the best way to deal with failure and setbacks may be to accept it, reframe it realistically and compassionately, and then have a good laugh about it.
Definition of Resilience: the ability to become strong, healthy, or successful again after something bad happens
What is Resilience?
 Resilience is the process of adapting positively in the face of adversity, trauma, tragedy, threats or significant sources of stress — such as family and relationship problems, health problems or workplace and financial stressors. It means “bouncing back” from difficult experiences.
Resilience is the process of adapting positively in the face of adversity, trauma, tragedy, threats or significant sources of stress — such as family and relationship problems, health problems or workplace and financial stressors. It means “bouncing back” from difficult experiences.
Being resilient does not mean that you don’t experience difficulty or distress. Emotional pain and sadness are common if you have suffered a major adversity or trauma in your life. In fact, the road to resilience is likely to involve considerable emotional distress. Many people suffer adverse events and have come out stronger as a result but that can be hard to see when you are in the midst of suffering.
Factors in Resilience
Resilience is not a trait that you either have or do not have. It involves behaviors, thoughts and actions that can be learned and developed in anyone. A combination of factors contributes to resilience. Many studies show that the primary factor in resilience is having caring and supportive relationships within and outside the family. Relationships that create love and trust, provide role models and offer encouragement and reassurance help bolster a person’s resilience. Several additional factors are associated with resilience:
- A positive view of yourself and confidence in your strengths and abilities.
- The capacity to make realistic plans and take steps to carry them out.
- Skills in communication and problem solving.
- The capacity to manage strong feelings and impulses.
 7 ways to build resilience
7 ways to build resilience
- Connect with others. Form good relationships with close family members, friends and others. Accept help and support from those who care about you and will listen to you. Being active in community groups and church, temple or synagogue and volunteering to help other less fortunate can provide social support and help you with reclaiming hope.
- Take care of yourself. Pay attention to your own needs and feelings. Engage in activities you enjoy and find relaxing. Exercise regularly. Develop confidence in your ability to solve problems and trust your instincts. Taking care of yourself helps to keep your mind and body primed to deal with situations that require resilience.
- Keep things in perspective. Even when facing very painful events, try to consider the stressful situation in a broader context and keep a long-term perspective. Avoid blowing the event out of proportion and seeing crises as insurmountable problems. You can’t change the fact that highly stressful events happen, but you can change how you interpret and respond to these events.
- Move toward your goals. Develop some realistic goals. Do something regularly — even if it seems like a small accomplishment — that enables you to move toward your goals. Accept circumstances that cannot be changed and focus on situations you can alter. Instead of focusing on tasks that seem unachievable, ask yourself, “What’s one thing I know I can accomplish today that helps me move in the direction I want to go?”
- Take positive, decisive actions. You probably have more influence that you think. Take action in the face of negative situations as much as you can, rather than detaching completely from problems and stresses and wishing they would just go away.
- Find opportunities for growth. People often learn something about themselves and may find that they have grown in some respect as a result of their struggle with loss. Many people who have experienced tragedies and hardship have reported better relationships, greater sense of strength even while feeling vulnerable, increased sense of self-worth, a more developed spirituality and heightened appreciation for life.
- Maintain a hopeful outlook. An optimistic outlook enables you to expect that good things will happen in your life. Try visualizing what you want, rather than worrying about what you fear. Try looking beyond the present to how future circumstances may be a little better. Note any subtle ways in which you might already feel somewhat better as you deal with difficult situations.
Get Started with Building your Resilience Muscle
Resilience is the ability to bounce back from tough situations and to avoid becoming a victim of helplessness. Being resilient can help you manage stress, lower your chances of depression, and it has even been proven to help people live longer. You may feel like you’ve had so much bad luck that it’s impossible to come out strong. Once you learn to seize your life by the reins and prepare for the unexpected, you’ll be on your way to being a more resilient person — and to living a happier, more purpose-filled life as a result. Use the steps above to get started.
OCD Treatment for Children and Teenagers
 I just had the honor of attending the OCD Foundation’s first-ever Behavior Therapy Training Institute on Pediatric OCD, which was held at Rogers Memorial Hospital in Wisconsin in mid-September. The treatment for children and teens with OCD is not all that different from adults. The main components of OCD treatment include:
I just had the honor of attending the OCD Foundation’s first-ever Behavior Therapy Training Institute on Pediatric OCD, which was held at Rogers Memorial Hospital in Wisconsin in mid-September. The treatment for children and teens with OCD is not all that different from adults. The main components of OCD treatment include:
- Education/Rapport Building (what is OCD? building the client’s trust)
- Cognitive Therapy (motivation, naming and externalizing the OCD, responding to content vs themes, etc)
- Exposure and Response Prevention (identifying triggers and gradually exposing the child until anxiety declines)
- Family Therapy (teaching parents how to help their child)
- Contingency Management (setting up a reward plan to increase motivation)
- Relapse Prevention (what to do at the early signs of anxiety or stress)
While we do use cognitive strategies especially for motivation with children, we emphasize behavioral strategies even more with children. Children often aren’t able to articulate the thoughts driving their rituals. They may say “I don’t know” or “It just feels right” or “I can’t help it.” As children and teens mature, it may seem their OCD is becoming more sophisticated because they start attributing reasons to why they do things.
When we are assessing OCD in children, teens or adults, the process is the same. The therapist will be thinking about these factors:
- Triggers: What stimuli trigger the obsession?
- Obsession: What is the core fear?
- Compulsions: How does the person attempt to neutralize the obsession?
There are four main steps in designing a personalized OCD treatment program for your child or teen.
Step 1: Define the Obsessions and Select the First Target Obsession to Work on
First, we need to determine if the thought is an obsession. If your child has a strange or irrational thought and can dismiss it, it’s not an obsession. Normal people have intrusive thoughts but the difference is that people without OCD do not attribute much meaning to them. Most people just shrug it off as a strange thought and go on with their day.
People often confuse the obsessions associated with OCD with the worries associated with Generalized Anxiety Disorder. It’s a worry if the content focuses on everyday problems that cause stress. GAD often has the same obsessional, repetitive feel to it except the theme of the worries are about real problems happening in the child’s life such as school, health, friends or family issues. An obsession, in contrast, is an intrusive, repetitive thought with senseless content. In children, common obsessions include doing things repeatedly until it feels “just right,” bad thoughts about sex or violence, superstitious thinking, and irrational concern about germs.
Step 2: Identify the Obsessions/Triggers and related Compulsions
Next, we need to identify the compulsions (rituals) that go along with the obsessive thoughts and what triggers the obsessive-compulsive cycle. External triggers are easier to work with because they are things, people, places or situations that scare people and trigger the OCD cycle. The types of OCD that usually involve external triggers include contamination, just right/not right obsessions, and doubt and uncertainty
Internal triggers, on the other hand, are the thoughts themselves, usually about sex, violence and blasphemy. For a thought to be a trigger, the thought itself must be perceived by the person as being dangerous. There are two categories of thoughts that people perceive as being toxic: the fear that having the thought can make it happen and/or the fear that having thought means something bad about the person who is experiencing the thoughts.
Step 3: Develop the Exposure Hierarchy
Exposure and Response Prevention (ERP) is the gold standard for treating OCD in all age groups. ERP is teaching you and your child an approach to life. Your child will learn that when something makes him afraid, he will face it. He will learn to approach his fears systematically through the Exposure Hierarchy. To develop a hierarchy, we will identify all the internal and external triggers for the obsessions and rank order them by level of difficulty. We will then proceed by working with you and your child in baby steps to approach their fears. We’ll use the feeling thermometer to help your child rate the difficulty of tasks. We will ask the parent to serve as the child’s ERP coach to help remind your child to practice their exposures during the week.
Step 4: Identify Response Prevention Guidelines for the Compulsions
The final step is to identify the compulsions (rituals) and to develop Response Prevention Guidelines that sound like this:
“When I get urge to (do my ritual), I will resist the urge and do this instead: XYZ.”
There are two categories of compulsions: Behavioral vs. Mental. Behavioral compulsions are things you can see your child doing such as washing, checking, reassurance seeking, straightening, etc. Mental compulsions are done in the child’s head and you may not even know they are doing them. These include counting, praying, figuring things out, replacing bad thoughts with good thoughts and mental checking.
We also need to determine if the compulsions are non-functional vs dysfunctional. Non-functional compulsions (rituals) are behaviors have no function other than to reduce anxiety related to OCD anxiety. Since these are non-sensical behaviors (like tapping three times on a door), our treatment plan will focus on eliminating these behaviors entirely because they have no function.
Dysfunctional compulsions (rituals) are excesses of normal behavior. We can’t completely eliminate these behaviors because done in moderation, they are normal behaviors like normal washing normal checking and normal prayer. For these, we help your child develop new rules for normal behavior.
During planned daily exposure time there is a schedule and specific tasks to be completed each day. Planned exposure time is generally 30 min to one hour per day. We’ll teach your child to engage in the obsessive thought while resisting the urge to ritualize. We will teach them that “When I get urge to …., I will resist the urge and do this instead …” We will also do some cognitive restructuring work where your child will learn to accept and even welcome anxiety and uncertainty by purposely choosing to expose himself to his triggers, knowing this will trigger his obsessive thoughts and urges to neutralize the anxiety with rituals.
The rest of the day, the child is taught how to deal with spontaneous exposures, or when the obsessive thoughts are triggered outside of planned exposure time. Again, we will teach your child that “When I get urge to …., I will resist the urge and do this instead …” We will help him learn to try to resist doing the compulsion and to focus on what he needs to doing instead (doing homework, watching TV, listening to music, paying attention in class, talking with friends, etc). The child will also have a list of guidelines to follow for any dysfunctional compulsions he may have an urge to do.
The key to Exposure and Response Prevention is to be ready to face your fears and to do your homework every night. You and your child will learn to ride up and down the OCD anxiety hill and beat OCD.
Making Mindful Choices
What is Mood-Dependent Behavior?
 Mood-dependent behavior is when you act on a feeling or an urge without pausing to consider the consequences or whether the behavior is appropriate to the situation. Often, mood-dependent behaviors will feel automatic and like they happen too quickly for you to have a choice. Mood-dependent behaviors may seem out of your control and difficult to change because of the powerful underlying emotions and negative thoughts driving them.
Mood-dependent behavior is when you act on a feeling or an urge without pausing to consider the consequences or whether the behavior is appropriate to the situation. Often, mood-dependent behaviors will feel automatic and like they happen too quickly for you to have a choice. Mood-dependent behaviors may seem out of your control and difficult to change because of the powerful underlying emotions and negative thoughts driving them.
When you are engaging in a mood-dependent behavior, you are acting on your underlying emotional state. For example, if you feel depressed, you do not get out of bed or you cancel plans with friends. If you have a craving for ice cream, you eat a pint for dinner, even though you are trying to lose weight. If you are irritable, you snap at your kids for no real reason or you nit pic your partner until it turns into a full-blown argument. Later on, when the mood has passed, you may feel guilt and shame about your actions. In the moment, however, you acted on your emotions without thinking because it would have been too uncomfortable to pause and practice tolerating the discomfort of a craving or being present with a negative emotions. Instead, you chose an action that can instantly bring some relief to your emotion, such as distracting from the emotion or giving in to it. It feels better in the short run but hurts you in the medium to long term.
You are not doomed to a life of engaging in mood-dependent behaviors. Instead, you can learn to practice mindful, strategic behaviors that will help you with managing your emotions and directing your actions toward meaningful goals.
My emotions are too strong. I feel out of control. How can I make Mindful Choices?
Mindful, strategic behaviors involve increasing awareness of your emotional state in the present moment and responding to situations more deliberately. This means taking the time to pause and ask yourself if how you are about to respond in the moment is going to really get you what you want. Is what you are about to do going to move you in the direction of your valued-based goals and dreams, or is it a mood-dependent response that may be counterproductive to your most cherished goals? In other words, how likely is it that you are going to regret how you are about to act?
In order to engage in mindful, strategic behavior, try breaking down the situation into the following components:
- What is the environmental prompt? Exactly what is happening in the moment that is urging you to respond?
- What is your internal mood?
- What is your short-term objective/goal?
- What is your long-term objective/goal?
- What behavior (action) will lead to accomplishing your goal?
- If you choose to follow your mood in this moment, will it interfere with or enhance your objectives/goal attainment?
While this type of problem-solving may seem self-evident, consider how easy it is to slip into the habit of engaging in mood-dependent behavior instead of mindful behavior. Quite often, an intense emotional state makes it seem difficult, or even “impossible,” to mindfully choose alternate (mindful) behaviors. While it may feel this way in the moment, it is possible to choose mindful behavioral responses over mood-dependent ones. The trick is choosing to practice emotional regulation strategies and mindfulness practices with greater frequency, so that it becomes more natural to approach your mood states more deliberately.
Mood-Dependent Behavior
- Chosen entirely based on whatever your current mood happens to be.
- At the whim of your internal emotional state.
- Not mindfully chosen… reactive and impulsive.
- Little to no consideration for consequences/effects on other people.
Mindful Behavior
- Guided by your heartfelt values and goals.
- Intentional, deliberate, and strategic.
- Careful, thoughtful consideration given to future consequences and the effects on other people.
- Responsive, not reactive… using “wise mind.”
When you take a moment to reflect on how you typically respond to your emotional states in the moment, do you notice that you have a tendency to gravitate toward mood-dependent or mindful behaviors more often? Take the time to consider the consequences that various courses of action have on your well-being, relationships, and pursuit of your goals. If you believe that you may benefit from using mindfulness and emotion regulation coping skills, make a commitment to yourself that you will begin to integrate these practices into your daily life.
A great way to learn Mindfulness in as little as 10 minutes a day is through the Headpsace mindfulness program. Click here to Get Some Headspace. Just remember that mindfulness is a journey, not a destination. Be patient.
 When potential new clients call me, they often ask if cognitive behavior therapy (CBT) works and what the success rate is. I say, “It depends on your motivation level and whether you are willing to practice the skills in between sessions.”
When potential new clients call me, they often ask if cognitive behavior therapy (CBT) works and what the success rate is. I say, “It depends on your motivation level and whether you are willing to practice the skills in between sessions.”
Fitness for the Brain
CBT is fitness for the brain. There are many different skills you can learn, like mindfulness, awareness of emotions and thoughts, identifying thinking traps, realistic thinking, decatastrophizing, reducing vulnerability to negative emotions, and acceptance, to name just a few. You can pick up a self help book and learn what these skills are and how to do them by yourself. However, most people don’t. They want my guidance in how to apply these skills to their own situations.
CBT is Not Magic
Sometimes, however, people think there is a magic bullet. They hope if they visit a therapist’s office that the therapist will have a magical way to change their brain without them having to do anything differently. This isn’t how CBT works.
CBT is Active and Collaborative
CBT is a collaborative and active process whereby the therapist helps you to become aware of your thinking and behavioral patterns and, together, you and your therapist identify strategies and tools that can help. Then it is your job in between sessions to practice the skills everyday. You may only see your therapist for one hour a week but there are 167 additional hours in a week for you to practice your skills. Like with physical exercise, if you only workout once a week, your fitness level may improve but it will be limited. However, if you work out a little bit everyday, your fitness level will soar.
CBT Requires Practice
In CBT, “practice” refers to repeating a cognitive or behavioral skill again and again over time. It begins with the intentional rehearsal of the new skill. At this stage, practice is conscious and takes effort. It is not yet natural. You have to remember to use the skill and you may need to read a notecard or write things down in order to remember what to do. Later, as the skill becomes part of your memory, you may start to use the skill more naturally and unconsciously. The quality of your practice and your knowledge base will largely determine the outcome of each practice session.
The old adage that “practice makes perfect” is rarely true. It is very possible to practice the same skill repeatedly with no increase in achievement or accuracy of application. Think of the people you know who have been driving, cooking, or even teaching for many years with no improvement in their skills. Why is this? How is it possible for one to continually practice a skill with no resulting improvement in performance?
What Makes for Successful Practice?
For practice to improve performance, four conditions must be met:
1. You must be sufficiently motivated to want to improve performance. If you have not attached meaning to learning the new skill, then your motivation will be low.
2. You must have the knowledge necessary to understand the different ways that the new skill can be applied.
3. You must understand how to apply the new skill to deal with a specific situation.
4. You must be able to analyze the results of that application and know what needs to be changed to improve performance in the future.
Guided Practice Helps
Practice may not make perfect, but it does make permanent, thereby aiding in the retention of learning. Consequently, we want to ensure that you practice the new skill correctly from the beginning. Early practice that is done in the presence of a therapist (referred to as guided practice) can offer immediate and corrective feedback to help you analyze and improve your practice. When the practice is correct, the therapist can then assign independent practice (usually homework) in which you can rehearse the skill on your own to enhance learning and retention.
Short-Term and Long-Term Practice
Effective practice starts with massed practice for fast learning and proceeds to distributed practice over a longer term time frame for retention and automatic recall. Practicing a new skill during time periods that are very close together is called massed practice. This produces fast learning, as when one mentally rehearses a multiplication table. Immediate memory is involved here, and the information can fade in seconds if it is not rehearsed quickly. Cramming for an exam is an example of massed practice. Material can be quickly chunked into working memory, but can also be quickly dropped or forgotten if more sustained practice does not follow soon. This happens because the material has no further meaning, and thus the need for long-term retention disappears.
Sustained practice over time, called distributed practice, is the key to retention. If you want to remember a multiplication table later on, you will need to use it repeatedly over time. Thus, practice that is distributed over longer periods of time sustains meaning and consolidates the learnings into long-term storage in a form that will ensure accurate recall and applications in the future.
 I just got back from a three-day workshop at the Beck Institute in Philadelphia on Teaching and Supervising Staff in Cognitive Behavior Therapy. While the content of the workshop will help me improve the CBT staff training program at the CBT Center, the most invigorating part of the workshop was the opportunity to learn from the other participants. There were about 50 professors and expert CBT practitioners at this workshop from all around the world, including China, India, Japan, South Africa and Great Britain.
I just got back from a three-day workshop at the Beck Institute in Philadelphia on Teaching and Supervising Staff in Cognitive Behavior Therapy. While the content of the workshop will help me improve the CBT staff training program at the CBT Center, the most invigorating part of the workshop was the opportunity to learn from the other participants. There were about 50 professors and expert CBT practitioners at this workshop from all around the world, including China, India, Japan, South Africa and Great Britain.
I felt like I was “home” in a group of people who were just as excited about CBT as me and the life-changing impact CBT offers to our clients. Sitting there, I realized that these 50 people – me included – will be impacting thousands of lives, not only through our direct client care but, more importantly, by training other therapists in CBT. There continues to be a deficit in well-trained CBT therapists who actually practice evidence-based CBT and offer scientifically-based psychotherapy to their clients. The Beck Institute is going to develop a list serve and other ways for our group to stay connected over time. This was a pleasant surprise of attending the workshop. In addition, I made a few new friends with whom I hope to keep in touch.
By far, the highlight of the workshop was the opportunity to spend two hours with Dr. Aaron Beck. For a CBT therapist, this is like having a meeting with Freud. Dr. Beck is credited as the father of cognitive behavior therapy and has done more than any other single individual to disseminate evidence-based therapy. Dr. Beck talked to us about the past and future of CBT. He said in the early days of CBT, he felt very lonely since other schools of psychotherapy were rejecting of CBT. He said talking to his teenage daughter, Judy, inspired him to go on with his research. By the way, Judy is now the leader of the Beck Institute and will carry on Dr. Beck’s work for the next generation.
Dr. Beck said, in the the future, he believes there will be one broad unifying theory of psychopathology but he still thinks there will be a variety of evidence-based treatments for different problems since different strategies need to be emphasized for different problems and client styles. He said therapists should base interventions on the overall psychological conceptualization of the individual client and then consider evidence-based strategies for specific disorders. Techniques need to be adapted to the case formulation and to patient’s learning capabilities. He told us to not be technique driven or beat a technique to death but, rather, have some variety in our treatment approaches and suit them to the client’s needs.
I feel like I am coming back from a spiritual journey to Mecca or Lourdes or the Holy Land. Every time I go to the Beck Institute, I am re-inspired for the work I do everyday with my clients and the staff at the CBT Center of Silicon Valley.
Self-soothing is a key part of self-care. The goal of self-soothing is to comfort yourself emotionally and physically by doing things that are sensually pleasant and not harmful. Self-soothing is a mindfulness practice when you are focusing your full attention on the feelings being experienced by your five senses. By being fully present on what you are experiencing in the moment, you will be able to get you outside of your head and away from troubling thoughts, feelings, and impulses.
Here are some ideas on how you can practice self-soothing this summer.
Vision: Plant some bright flowers in your garden. Go on a hike and notice the trees and flowers. Watch the stars on a clear summer night. Attend a summer art festival.
Hearing: Listen to music at an outdoor concert. Go to the beach and hear the sounds of the ocean. Listen to the crackling of firecrackers at a Fourth of July festival.
Smell: Buy some flowers with vibrant fragrances at the Framer’s Market. Take in the savory smells at a barbecue this summer. Bake an apple pie.
Taste: Sample some summertime fruits. Mindfully eat an ice cream or a popsicle. Sip a cold smoothie. Let a piece of dark chocolate melt in your mouth.
Touch: Soak your feet in the pool. Walk barefoot in the sand at the beach. Apply suntan lotion to your skin. Feel the heat of the sun on your body.
The New York Times recently published an article that examines the difference between evidence-based CBT and what they call the “dim sum” approach, which is the eclectic approach many therapists use when they integrate strategies from a variety of different types of therapies. Here’s a quote from the article:
“CBT refers to a number of structured, directive types of psychotherapy that focus on the thoughts behind a patient’s feelings and that often include exposure therapy and other activities. Instead, many patients are subjected to a kind of dim-sum approach — a little of this, a little of that, much of it derived more from the therapist’s biases and training than from the latest research findings. And even professionals who claim to use evidence-based treatments rarely do.”
Read the full article here: Looking for Evidence that Therapy Works New York Times 3-25-13
So, how do you know if your therapist is really practicing evidence-based CBT? Here are some ways to know the difference:
- Is your therapist goal-oriented or does he/she focus on issues that seem unrelated to your problem(s)?
- Does your therapist track your mood and other relevant factors to see if you are improving?
- Does your therapist work with you to develop a cognitive-behavioral formulation of your problem(s)?
- Do you understand the factors that are maintaining your problem(s) and do you and your therapist have a treatment plan to impact those factors?
- Has your therapist read the treatment manuals for your particular problem?
- Does your therapist regularly assign homework and follow up on it?
- Is your therapist active and collaborative during the session or does he/she mainly listen?
- Does your therapist regularly use CBT techniques such as teaching you how to examine your thinking patterns and helping you engage in behavioral experiments and exposures?
- Is your therapist compassionate and attentive yet directive and solution-focused?
Your therapist may not do all of the above every time but you should be able to answer yes to the majority of the above questions most of the time.
About the Cognitive Behavior Therapy Center of Silicon Valley
The mission of the Cognitive Behavior Therapy Center of Silicon Valley is to offer evidence-based therapy for adults, children and teenagers with anxiety, obsessive compulsive disorder and eating disorders. The Center’s primary focus is on the evidence-based treatment of anxiety and related disorders because there are subtle differences in how each disorder should be treated. While many therapists work with anxiety disorders, the cognitive and behavioral approaches used at the CBT Center require extensive continuing education in the specific conceptualization for each person and evidence-based strategies for each disorder.
Laura Johnson, Center Director and Certified Cognitive Therapist, started the Cognitive Behavior Therapy Center because there is a lack of therapists in the South Bay who are trained to deliver evidence-based cognitive-behavioral treatments for anxiety, OCD and eating disorders. Currently, we have several therapists at the Cognitive Behavior Therapy Center. All therapists at the Cognitive Behavior Therapy Center are employees of the Center and receive extensive training in CBT and other evidence-based therapies. This ensures that you will receive high quality CBT no matter which therapist you see at our Center.
 Are You Focused on Learning to Be The Best or Trying to Prove You Already Are?
Are You Focused on Learning to Be The Best or Trying to Prove You Already Are?
“Be Good” goals are about proving yourself (being good). When you are striving to “be good,” you are focused on showing yourself and others that you are already completely competent. You are focused on the end result of your performance and showing everyone that you are already the best at whatever you are doing. Mistakes are awful because they contradict the image of yourself as perfect. In contrast, “Get Better” goals are about improving yourself (getting better). When you are focused on getting better, you are interested in learning and growth. You are okay with making mistakes because you know that you don’t know everything. Mistakes are seen as opportunities to learn.
“Being Good” Works When Times are Good
Wanting to “be good” is very motivating and can lead to excellent performance, provided that things don’t get too difficult, according to Heidi Halvorson PhD, author of Succeed. Unfortunately, she says, when the road gets rocky, people who are focused on proving themselves tend to conclude that they don’t have what it takes and give up too soon.
“Getting Better” is Better When You Face Challenges
When we focus on getting better, we take face difficulty with greater calm and use the experience from our learnings to fuel our improvement. Halvorson has found that people who pursue growth often turn in the best performances because they are more resilient in the face of challenges.
“Getting Better” Helps You Enjoy the Journey
 When your goal is to get better rather than to be good, you tend to enjoy what you’re doing more and find it more interesting. In other words, you appreciate the journey as much as the destination, says Halvorson. You also engage in deeper, more meaningful processing of information and better planning for the future. You are even more likely to ask for help when you need it, and more likely to truly benefit from it.
When your goal is to get better rather than to be good, you tend to enjoy what you’re doing more and find it more interesting. In other words, you appreciate the journey as much as the destination, says Halvorson. You also engage in deeper, more meaningful processing of information and better planning for the future. You are even more likely to ask for help when you need it, and more likely to truly benefit from it.
“Getting Better” Reduces Anxiety and Depression
If your goals are more about self-growth than self-validation, you will be able to deal with depression and anxiety in more productive ways. Feeling bad will make you get up and take action to solve your problems, rather than just lie around and feel sorry for yourself. Not surprisingly, you will be less depressed than other people who are constantly trying to prove they are capable and worthy, says Halvorson.
Try to Focus on “Getting Better”
The bottom line is, whenever possible, try to turn your goals from being good to getting better. Rather than complain about all the ways in which you, your job or your relationships aren’t perfect, focus on all the ways in which they are going well and can be improved. At work and at school, focus on expanding your skills and taking on new challenges rather than impressing everyone with how smart and knowledgeable you are. When your emphasis is on what there is to learn rather than what there is to prove, you will be a lot happier and will achieve a lot more.
Adapted from Succeed: How We Can Reach Our Goals by Heidi Halvorson PhD (2010).
Baby Steps Can Lead You Down the Road of Success.
 Set smaller goals and get bigger results? This might seem counterintuitive to you. And if it does, you are not alone. We’re all used to hearing about stretch goals, and when you feel empowered, stretch goals are inspiring and motivating. But when you feel overwhelmed, stretch goals can create paralysis and result in procrastination. When you set your goals too high, you might find it overwhelming and too time consuming. You just give up or keep on changing your goals instead of slowly and steadily working through the baby steps to a bigger goal.
Set smaller goals and get bigger results? This might seem counterintuitive to you. And if it does, you are not alone. We’re all used to hearing about stretch goals, and when you feel empowered, stretch goals are inspiring and motivating. But when you feel overwhelmed, stretch goals can create paralysis and result in procrastination. When you set your goals too high, you might find it overwhelming and too time consuming. You just give up or keep on changing your goals instead of slowly and steadily working through the baby steps to a bigger goal.
Setting small goals makes sense from a more-likely-to-succeed perspective. Baby steps help us manage the fear that keeps us from doing the tasks we dislike or that seem too hard. You feel more confident pursuing smaller goals because you know you are going to achieve them. So you do and this soon puts bigger goals within reach. Setting and reaching small goals sets up a positive snowball effect. Small goals will give you small successes and that will motivate you to continue.
Keep in mind that goal setting isn’t all about success – there will be setbacks. You need to anticipate failure (like gaining a pound after you’ve lost two), so you don’t end up getting derailed and quitting. This is why small goals are preferable because you can measure achievement and the setbacks don’t knock you down so harshly.
When you give up early, it’s likely your goals were too big in the first place. Most people never reach their biggest goals because they can’t stick to them in the beginning. The first 30 to 60 days are key to long term success. That is when you are more likely to put in the hard work to get to a new or different result. You need to put in twice the work in the beginning because you are starting a new habit and breaking an old one at the same time.
The key is to start small with baby steps, achieve some early wins and build your confidence to keep moving forward. When you set small goals, three powerful things happen:
- You achieve the small goals on your list pretty quickly.
- You see yourself making regular progress and this is reinforcing.
- You gain the courage to pursue bigger goals and you keep on working.
Reaching a big goal involves conquering a series of smaller goals. If you’ve tried to reach big goals in the past and failed, don’t give up. Try re-starting this year with smaller goals using the following steps:
 Dream big, execute small. Figure out what it is you want to accomplish. Pick something that is really important to you. Identify why you want to accomplish this goal and what benefits it will have for you. This might be a big long-term goal, but it can help get you started with setting your short-term, smaller goals.
Dream big, execute small. Figure out what it is you want to accomplish. Pick something that is really important to you. Identify why you want to accomplish this goal and what benefits it will have for you. This might be a big long-term goal, but it can help get you started with setting your short-term, smaller goals.- Break up your major goal into smaller, more manageable parts. You are more likely to make your dream come true this way. If your big goal is to walk/jog a half-marathon in September, break it down into baby steps. The small steps could be walk around the block three times this week, hike half a mile walk with my partner, jog one block, etc. Before you know it, you’ll be jogging around the high school track and feeling really good about yourself.
- Stay focused on the present. If your brain starts thinking about the big goal that is 6 months or a year into the future, you will start feeling overwhelmed and fearful or you may have negative thoughts that make you feel like giving up. Instead, use mindfulness to bring your brain back to the small goal that you can realistically achieve in the short-term. Remember, even the highest achievers started with small steps.
- Be positive. Say “I will” rather than “I won’t.” Negative goals make you feel deprived instead of making you feel good about your successes. Instead of saying, “I won’t eat chocolate,” tell yourself, “I will eat vegetables with dinner.”
- Make goals short term and specific. Most small goals can have a set deadline or at least a general timeframe. Specify exactly what you plan to do by tomorrow or next week. Say “I’m going to walk 15 minutes after dinner two evenings this week,” rather than “I’m going to exercise.”
- Measure and track. Use a calendar to track your progress in a visible way. Write down and check off every time you complete a small goal. At the end of the month, you will be surprised and proud at how much you got done.
- Be realistic. Set a realistic amount of small goals. Even small goals take time and effort. In order to achieve long-term success, you have to find small goals you can live with and incorporate into your daily schedule.
- Celebrate and reward yourself. Recognize each small victory. They are your building blocks for long-term success. Sometimes people don’t feel worthy of celebrating a small achievement. You might say, “That was no big deal,” or “It was too easy.” However, you are more likely to stay motivated if you think positive and recognize small successes.
Good luck reaching your goals this year. Make 2013 the year of small goals with big results.
 In July, I had the privilege of traveling to Chicago to observe a two-day intensive live Anxiety & OCD treatment group led by Reid Wilson, Ph.D. There were eight people in the group with anxiety and OCD, many of whom had been suffering for years with chronic anxiety, panic, social anxiety, depression, obsessive thoughts, mental rituals and/or compulsive behaviors. I was skeptical the morning of the first day. Reid Wilson was making some big claims like “You will need to trust me. You can listen and think you will work on it later…and you will fail. Or you can listen and act – today – and begin your healing.” Given the severity of this group’s long-standing problems with anxiety and OCD, I didn’t believe that these folks could achieve significant progress by the end of a two-day, 16 hour treatment group. Boy was I wrong!
In July, I had the privilege of traveling to Chicago to observe a two-day intensive live Anxiety & OCD treatment group led by Reid Wilson, Ph.D. There were eight people in the group with anxiety and OCD, many of whom had been suffering for years with chronic anxiety, panic, social anxiety, depression, obsessive thoughts, mental rituals and/or compulsive behaviors. I was skeptical the morning of the first day. Reid Wilson was making some big claims like “You will need to trust me. You can listen and think you will work on it later…and you will fail. Or you can listen and act – today – and begin your healing.” Given the severity of this group’s long-standing problems with anxiety and OCD, I didn’t believe that these folks could achieve significant progress by the end of a two-day, 16 hour treatment group. Boy was I wrong!
Steps To Playing the Anxiety Mental Game
Dr. Wilson spent the first four hours introducing the concepts behind the Anxiety Mental Game and enhancing motivation to play the game. He said, “You have OCD or Anxiety. You’ve been working on it, struggling with it, worrying about it, trying to control it, and you haven’t won yet.” Dr. Wilson said the only way to win against anxiety is to follow some paradoxically absurd strategies. He outlined three steps:
- The first step is to identify how anxiety is ruining your life and to identify how your future will be different if you face your fears. This step creates your reason or motivation for wanting to play this game. You need to have a compelling reason because this game is hard.
- The second step is to understand the principles behind playing the anxiety game. You need to be able to gain a mental shift from “I must avoid anxiety at all costs” to “I want to seek out anxiety (frequency), I want it to be strong (intensity), and I want it to last (duration).” And you need to learn that “whatever happens, I can handle it.”
- The third step is to provoke anxiety. Instead of avoiding, resisting or simply tolerating anxiety (which is where anxiety wins), you need to proactively invite more anxiety into your daily life. This means being able to genuinely believe and tell yourself, “I really want anxiety to keep happening. I win if it keeps happening” and then to go out and actually create opportunities (called “exposures” or “behavioral experiments”) to feel anxious.
You might be thinking, “I am already doing the things that make me anxious. How can doing more of them help?” The difference is you are probably muscling through your daily life if you aren’t actively avoiding. You are probably telling yourself, “This is uncomfortable. My anxiety is unbearable. I can’t handle this anymore. I need relief from anxiety.” And you might go into anxiety-provoking situations with some subtle safety behaviors to try to protect yourself, like over-preparing, not talking, leaving early, sitting in a place where you won’t be noticed or distracting yourself during the situation.
Preparing to Play The Anxiety Mental Game
To prepare for the Anxiety Mental Game, the group members were asked to identify and review their hierarchy of anxiety-provoking content and to pick one item that they would practice experiencing at lunch time. Every time the group member could enthusiastically say things to themselves when they felt anxious like “Excellent! Just what I wanted,” or “I can handle this,” or “Give me your best shot. I want my life back,” they would get a point. Dr. Wilson gave each group member a clicker to keep track of their points. After lunch, they came back and reported on how many points they had accumulated. Some of the folks had 80+ points in just two hours!
In addition to the new self-talk, the participants were also coached about where to put their attention while they were playing the Anxiety Mental Game. Dr. Wilson said, “The problem is not what you think it is. The problem is not the content of your fears. The problem is where you put your attention. You will either pay attention to the content (i.e. your list of anxiety-provoking fears, worries and other negative thoughts) or you will pay attention to anything else. You will decide – moment by moment. You have to choose to withdraw your attention from your content. That is your job here.”
Rules for Winning the Anxiety Mental Game
 The way to win the Anxiety Mental Game is to change your frame of reference from “This is serious and dangerous” to “This is a mental game.” The new rules you need to learn are:
The way to win the Anxiety Mental Game is to change your frame of reference from “This is serious and dangerous” to “This is a mental game.” The new rules you need to learn are:
- Do not pay attention to your content.
- Accept obsessive and anxious thoughts when they pop up.
- Want to make yourself uncertain about the content.
- Want to be anxious and stay anxious.
- If necessary, make rules and follow them (to get you through the exposures).
By the end of the two-day treatment group, all the group members reported some amount of reduction in their anxiety and fears. Through the exposures, they learned that “This is hard and I want it” and “I can handle this.” By observing the group members’ improvements, I became a believer in the power of playing this mental game to beat anxiety and OCD.
You can listen to Reid Wilson talking about the Anxiety Mental Game by clicking to listen to this Anxiety Mental Game podcast. If you are interested in learning to play the Anxiety Mental Game, call us at (408) 384-8404 to set up an appointment with one of our therapists.
Cognitive Behavior Therapy Center Opens in Convenient West Valley Location
The Cognitive Behavior Therapy Center, Adult & Child Counseling Inc. is a professional corporation providing evidence based treatments for anxiety, OCD and related issues such as eating and sleep problems.
“I opened this Center because there is a great need for places where consumers can get real cognitive behavior therapy in the Bay Area. CBT is the most widely researched therapy in the world, yet very few therapists are trained to provide it in an effective manner.” – Laura Johnson, President of the Cognitive Behavior Therapy Center of Silicon Valley
Some of the hallmarks of the Cognitive Behavior Therapy Center of Silicon Valley include:
- Laura L.C. Johnson, its Founder and Director, is certified by the Academy of Cognitive Therapy, the only organization that certifies CBT therapists based on reviewing the therapist’s credentials, CBT training, session audiotapes and a case write-up.
- The Center uses a personalized yet scientific approach, basing the client’s therapy plan on what works in research with the individual needs of the client.
- The Center specializes in the evidence-based treatment of anxiety disorders, OCD spectrum disorders, eating disorders and anxiety-related sleep problems.
- The Center is centrally-located on the border of San Jose and Saratoga. From this central location, the Center serves the Silicon Valley communities of San Jose, Saratoga, Mountain View, Santa Clara, Sunnyvale, Los Gatos, Los Altos, Palo Alto, Cupertino, and Campbell, CA.
Copyright © 2024 All Rights Reserved