Cognitive Behavior Therapy 101
Often in our initial assessment appointment, a new client will ask “so what is Cognitive Behavior Therapy anyway?” Most people have read some about the disorder they are seeking help for and know that CBT is the treatment of choice, but CBT itself can be a mystery.
The CBT Viewpoint
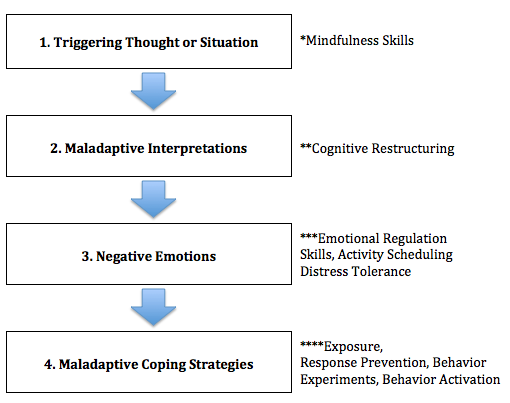
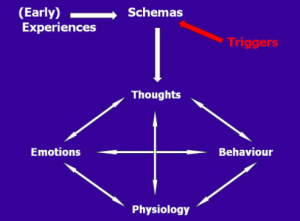
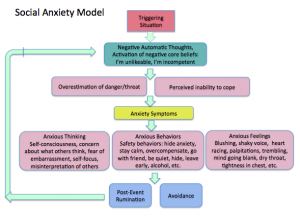
In order to understand what CBT treatment is like, you first need to understand how CBT views problems like anxiety, depression and OCD. There are four parts: the triggering thought or situation, unhelpful or inaccurate thoughts about that situation, negative emotions, and maladaptive coping strategies. Here is the cycle illustrated with two examples:
Maladaptive coping strategies don’t work because they only relieve your negative feelings in the short term and keep you from learning anything new about the triggering situations. These behaviors end up reinforcing your unhelpful thoughts and the cycle continues.
CBT Strategies
Once you understand how CBT view problems, and apply it to the difficulties in your own life, you are ready to look for solutions. There are skills that can help you in each stage of the CBT cycle. No one strategy will work for everyone, but once you acquire some that work for you, you can start to unhook yourself from the cycle and new, healthier patterns develop.
* For the triggering thought or situation we teach mindfulness skills. Here the important thing to do is learn to notice your triggers in an objective non-judgmental way. For example, in the case above of the person having anxiety about giving a speech, we might teach her to notice when the thoughts and feelings creep up and say things like “I’m noticing more worries about this speech”. The key with mindfulness is to notice your symptoms without trying to change them. This nonjudgmental perspective sets the stage for the strategies that come next.
** Next comes cognitive restructuring. Our thoughts have strong effects on how we feel but just because we think something, doesn’t make it true. Cognitive restructuring involves learning to evaluate our thoughts for accuracy and helpfulness and, when we find a thought that is inaccurate or unhelpful, we replace it with something that helps us to see the situation more clearly and to act in accordance with our values.
*** Some of the strategies we use to cope with unpleasant emotions are emotional regulation skills, distress tolerance and activity scheduling. These strategies are aimed at helping you cope with an unpleasant emotions even if you can’t change them.
**** This last category involves changing our behavior response when faces with negative emotions. Often it involves doing the opposite of what our thoughts and feelings try to convince us to do. With behavioral activation, we schedule potentially rewarding and productive activities into the day to break an avoidant cycle. Exposure involves being in a feared situation without trying to escape or avoid feeling anxious. Behavior experiments involve testing out beliefs about ourselves and the world instead of assuming that our thoughts are true.
How to Get CBT for Anxiety and OCD Disorders in San Jose/Los Gatos and Sacramento/Roseville
The Cognitive Behavior Therapy Center specializes in therapy and counseling with adults, children and teenagers. Click to send an email for more information on how we can help you or your family members improve your outlook.
Silicon Valley and Sacramento Valley Communities We Serve
Cognitive Behavior Therapy Center of Silicon Valley offers evidence-based therapy for Anxiety and Obsessive Compulsive Disorder near the following Silicon Valley/San Jose communities:
San Jose Therapy Counseling • Saratoga Therapy Counseling • Los Gatos Therapy Counseling • Monte Sereno Therapy Counseling • Cupertino Therapy Counseling • Campbell Therapy Counseling • Mountain View Therapy Counseling • Los Altos Therapy Counseling • Sunnyvale Therapy Counseling • Santa Clara Therapy Counseling
Cognitive Behavior Therapy Center of Sacramento Valley offers evidence-based therapy for Anxiety and Obsessive Compulsive Disorder (OCD) near the following Sacramento Valley and Sierra communities:
Sacramento Therapy Counseling • Roseville Therapy Counseling • Rocklin Therapy Counseling • Granite Bay Therapy Counseling • Lincoln Therapy Counseling • Folsom Therapy Counseling • Citrus Heights Therapy Counseling • El Dorado Hills Therapy Counseling • Loomis Therapy Counseling • Grass Valley Therapy Counseling • Auburn Therapy Counseling
CONTACT US